Archive \ Volume.11 2020 Issue 4
Anxiety among COVID-19 Physicians during the Pandemic in the Health Care Center of the Rural Region
Fahad Jibran Siyal1*, Zahid Ali Shaikh2, Syed Zaryab Ahmed3, Moazzam Ali Shahid4, Faiza Agha5, MirHassan Khoso6, Ayaz Ali Unar1, Khalida Unar7, Raheela Saleem8, Muhammad Parial Shahani9
1 Institute of Pharmacy, Shaheed Mohtarma Benazir Bhutto Medical University Larkana, Pakistan. 2 Department of Medicine, ShaheedMohtarma Benazir Bhutto Medical University Larkana, Pakistan.3 Department of Biochemistry, Ziauddin University Karachi, Pakistan. 4 Department of Research, Ziauddin University Karachi, Pakistan. 5 Department of Biochemistry, Liquat National Medical College Karachi, Pakistan. 6 Department of Biochemistry, Shaheed Mohtarma Benazir Bhutto Medical University Larkana, Pakistan.7 Institute of Microbiology, Shah Abdul Latif University, Khairpur,Sindh, Pakistan.8 College of Pharmacy, Liaquat University of Medical and Health Sciences, Pakistan. 9 Department of Community Medicine, Shaheed Mohtarma Benazir Bhutto Medical University Larkana, Pakistan.
Abstract
Introduction: The COVID-19 pandemic is likely to put healthcare professionals in critical circumstances globally, having to make intolerable assessments and work under extreme pressures. It is very difficult to provide care for all severely sick patients with reserved resources. This may affect a physician’s mental health. Healthcare professionals are at greater risk of mental health concerns because they are allocating with tasks of the COVID-19 pandemic situation especially in rural areas where it is difficult to deal with uneducated attendants and patients. This study aims to assess the work pattern of doctors who are performing duties with COVID -19 patients. Results: A total of 33 doctors participated in this survey out of which the majority of the age group was found to be 27. In this survey 23 males (70%) and 10 females (30%) participated. 7 doctors (21.2%) were normal and they were not having anxiety, 12 of doctors (36.4%) were mild anxious, 8 doctors (24.2%) were moderate anxious, 6 doctors (18.2%) were having severe anxiety. Five males were normal, 6 males were mild anxious,7 males were moderate anxious and 5 males were severely anxious, and 2 females were normal, 6 females were mild anxious, 1 female was moderate anxious and 1 female was severely anxious. Conclusion: In this study, we found that those doctors who performed duty with COVID 19 patients were more worried when assessed with the GAD-7 scale.
Keywords: Anxiety, COVID-19, Physicians, Surveys and Questionnaires
INTRODUCTION
The COVID-19 pandemic is likely to put healthcare professionals in critical circumstances globally, having to make intolerable assessments and work under extreme pressures. It is very difficult to provide care for all severely sick patients with reserved resources. This may affect a physician’s mental health [1].In a survey it is found that physicians and nurses in hospitals have greater depression, anxiety caring health care workers is an important component of public health [2]. COVID-19 pandemic signifies a foremost challenge to our health systems around the world. Clinicians should have proper care wit PPE for the prevention of virus spread and ensure the best protection and mental health care to reserve their psychological and physical integrity [3]. In another study, it is important to develop some intervention programs and support approaches for the period of the COVID-19 pandemic to protect mental health and increase psychological resilience [4].Recent studies in China establish that the anxiety and depression present in both the general public and front-line nurses [5]. Last up to April 2020, not only patients but also 100 Physicians and 26 nursing staff died of COVID-19 in Italy. Health care professionals are more exposed to the risk of infection with diseased patients and it is due to the stressful work with unlimited time and the possible unavailability of PPE [6].Anxiety disorders are the most prevalent psychiatric disorders and are associated with a high burden of illness [7].Healthcare professionals are at greater risk of mental health concerns because they are allocating with tasks of the COVID-19 pandemic situation especially in rural areas where it is difficult to deal with uneducated attendants and patients. This study aims to assess the work pattern of doctors who are performing duties with COVID -19 patients.
MATERIAL AND METHODS:
The study is a cross-sectional hospital-based survey conducted via an online questionnaire that was developed through Google forms. In that GAD-7 form, anxiety was assessed with the scale based on a score with a minimum of 0 to a maximum of 21 [8]. The questionnaire was formed with the consultation of the epidemiologist and later it was sent to the concerned duty doctors. A total of 33 doctors were included in this study who were performing their duties with COVID-19 positive patients.
RESULTS:
A total of thirty-three (33) doctors participated in this survey out of which the majority of the age group was found to be 27 and it was about 30.3% as showed in Table No.1. In this survey, 70% (23) males and 30% (10) females participated as showed in figure No.1 (Gender). According to Table No.2 i.e. 21.2 % (7) doctors were normal and they were not having anxiety, 36.4% (12) of doctors were mild anxious, 24.2% (8) were moderate anxious 18.2% (6) were having severe anxiety. According to table No.3 i.e. 5 males were normal, 6 males were mild anxious,7 males were moderate anxious and 5 males were severely anxious, and 2 females were normal, 6 females were mild anxious, 1 female was moderate anxious and 1 female was severely anxious.
|
Table 1: Age Groups |
||
|
Age |
Frequency |
Percent |
|
24 |
1 |
3 |
|
25 |
3 |
9.1 |
|
26 |
4 |
12.1 |
|
27 |
10 |
30.3 |
|
28 |
4 |
12.1 |
|
29 |
3 |
9.1 |
|
30 |
2 |
6.1 |
|
31 |
3 |
9.1 |
|
32 |
1 |
3 |
|
33 |
2 |
6.1 |
|
Total |
33 |
100 |
Gender
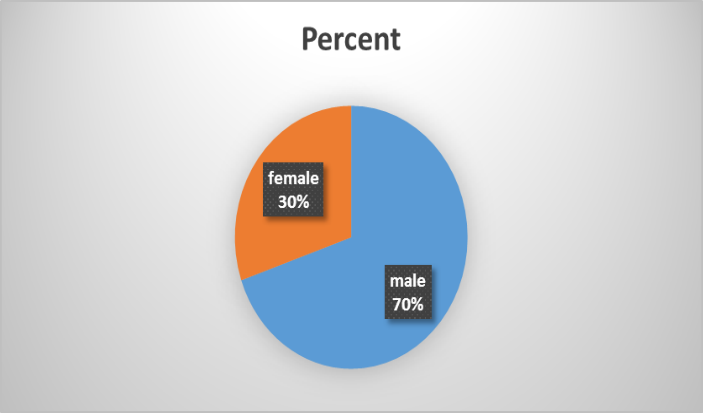
Figure 1, Genders of participated doctors.
|
Table 2: Scales of Anxiety |
|||
|
Frequency |
Percentage |
||
|
normal |
7 |
21.2 |
|
|
Anxiety |
Mild |
12 |
36.4 |
|
moderate |
8 |
24.2 |
|
|
Severe |
6 |
18.2 |
|
|
Total |
33 |
100 |
|
|
Table 3: GAD7ANX |
||||||
|
GAD7ANX |
Total |
|||||
|
normal |
mild |
moderate |
severe |
|||
|
Sex |
Male |
5 |
6 |
7 |
5 |
23 |
|
female |
2 |
6 |
1 |
1 |
10 |
|
|
Total |
7 |
12 |
8 |
6 |
33 |
|
DISCUSSION:
In the past, research has shown that epidemics can have significant and variable psychological effects on individuals and can lead to the creation of new psychiatric symptoms or worsening of pre-existing diseases such as fear of becoming ill or dying, helplessness, the propensity to blame those who are ill, panic attacks and anxiety [9].Therefore, it is common for everyone to experience elevated levels of anxiety or depression in a global crisis such as the COVID 19 pandemic. However, it puts more risk on the Physicians and other front-line health care workers who have to strike a balance between caring for the affected patients and protecting themselves, their family members, and their loved ones [10]. To this end, the American medical association has announced resources for the physicians to cope with the increased level of distress and anxiety [11].A limited number of studies have been conducted worldwide to evaluate the anxiety level in physicians and health care professionals including countries like China, USA, Oman and Singapore [12-15].Our study group included 33 physicians from interior Sindh. The age range was from 24 years old to 33 years old. The median age was 28.5 years. It is comparable to a study donein Singapore where the median age was 30 years. It is normal in our country to achieve a medical degree by the age of 22 to 23 years. The majority of our participants were 27 years old. This is somewhat comparable to a study done by Lai et al among 1830 health care workers in 34 hospitals from 9 different states of China. Their study showed the second-highest number of Physicians in this age group. Their largest group comprised of age group 31 to 40 years [16].In our study majority of the physicians were males 70% as compared to females 30%. In a study by Lai, 45% were males and 55 % were females. In a study done by Abdullah et al in Oman, they had higher proportions of females in their group 60% as compared to males 40%. Similarly, a study conducted by Benjamin et al.[17] that reported Singapore had higher female gender participation and involvement 68 % as compared to males 32 %. The reason for these contradictory results can be due to multiple factors prevalent in our society and one of them is our socioeconomic differences. In Pakistan especially in rural areas due to the veil system majority of the females are not allowed to go and do outdoor work. Men are the bread earners and hence one of the reasons for higher prevalence. Secondly, the majority of females are not highly educated. So, the majority of them do not attain professional degrees related to the health care system. Another big reason for this gender disparity in poverty levels in Pakistan as enlisted by Insiya Syed in her research topic “Shall I Feed My Daughter or Educate Her” [18]. In her article few other reasons mentioned are the Lack of investment in education by government, High cost of education, poor quality of education, No enforcement of compulsory education, social norms and insecurity, etc. In our study,the majority of the participants expressed mild anxiety as compared to no anxiety, moderate anxiety, or severe anxiety which had almost equal proportions. Jainbo Lai et al researched 1257 physicians and nurses from 34 different hospitals in multiple regions of China taking care of patients suffering from COVID 19. One of their assessment factors in mental health was anxiety besides other parameters like depression, sleep deprivation, etc. Their study also showed that among the anxiety group participants mostly had mild anxiety 29 % as compared to moderate and severe. This is comparable to our study. Our study is also comparable to another study where they included 1853 doctors from 348 hospitals of 31 different provinces of mainland China [19].Their frequency of mild, moderate, and severe anxiety was 68.0%, 19.0%, and 13.6% respectively indicating the majority of the subjects lying in the mild anxious state.This is supported by other studies as well [20].
CONCLUSION:
In our study, we found out that those doctors who have performed duty with COVID 19 patients tend me more anxious according to GAD 7 scale when compared to performing duty without COVID-19 patients.
REFERENCES
- Greenberg N, Docherty M, Gnanapragasam S, Wessely S. Managing mental health challenges faced by healthcare workers during COVID-19 pandemic. bmj. 2020 Mar 26;368.
- Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, Wu J, Du H, Chen T, Li R, Tan H. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA network open. 2020 Mar 2;3(3):e203976-.
- Denis M, Vandeweerd V, Van der Vliet D. COVID-19 Version: dd. 20 APR 2020 Transdisciplinary Insights - Living Paper
- Bakioğlu F, Korkmaz O, Ercan H. Fear of COVID-19 and Positivity: Mediating Role of Intolerance of Uncertainty, Depression, Anxiety, and Stress. International Journal of Mental Health and Addiction. 2020 May 31:1.
- Li Z, Ge J, Yang M, Feng J, Qiao M, Jiang R, Bi J, Zhan G, Xu X, Wang L, Zhou Q. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain, behavior, and immunity. 2020 Mar 10.
- Zhang Z., Liu S., Xiang M. Protecting healthcare personnel from 2019-nCoV infection risks: lessons and suggestions. Front Med. 2020 DOI: 10.1007/s11684-020-0765-x. [e-pub ahead of print] Accessed April 5, 2020.
- Chisholm D., Sweeny K., Sheehan P., et al Scaling-up treatment of depression and anxiety: a global return on investment analysis. Lancet Psychiatry. 2016;3(5):415–424.
- Löwe B, Wahl I, Rose M, Spitzer C, Glaesmer H, Wingenfeld K, Schneider A, Brähler E. A 4-item measure of depression and anxiety: validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. Journal of affective disorders. 2010 Apr 1;122(1-2):86-95.
- [Internet]. 2020 [cited 30 September 2020]. Available from: https://www.ama-assn.org/press-center/press-releases/new-ama-resources-help-combat-physician-stress-amidst-pandemic.
- 2020 [cited 25 September 2020]. Available from https://www.ama-assn.org/delivering-care/public-health/managing-mental-health-during-covid-19)
- [Internet]. 2020 [cited 25 September 2020]. Available from: https://www.ama-assn.org/delivering-care/public-health/managing-mental-health-during-covid-19).
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17(5):E1729.
- Xiao H., Zhang Y., Kong D., Li S., Yang N. The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med. Sci. Monit. 2020;26
- Li Z., Ge J., Yang M., Feng J., Qiao M., Jiang R., Bi J., Zhan G., Xu X., Wang L., Zhou Q., Zhou C., Pan Y., Liu S., Zhang H., Yang J., Zhu B., Hu Y., Hashimoto K., Jia Y., Wang H., Wang R., Liu C., Yang C. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain Behav. Immun. 2020;10(20)
- Badahdah AM, Khamis F, Al Mahyijari N. The psychological well-being of physicians during COVID-19 outbreak in Oman. Psychiatry Research. 2020 Jul;289:113053.
- Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, Wu J, Du H, Chen T, Li R, Tan H. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA network open. 2020 Mar 2;3(3):e203976-.
- Tan BY, Chew NW, Lee GK, Jing M, Goh Y, Yeo LL, Zhang K, Chin HK, Ahmad A, Khan FA, Shanmugam GN. Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Annals of Internal Medicine. 2020 Apr 6.
- [Internet]. 2020 [cited 25 September 2020]. Available from: https://www.ama-assn.org/delivering-care/public-health/managing-mental-health-during-covid-19)
- Liu CY, Yang YZ, Zhang XM, Xu X, Dou QL, Zhang WW, Cheng AS. The prevalence and influencing factors in anxiety in medical workers fighting COVID-19 in China: a cross-sectional survey. Epidemiology & Infection. 2020 Jan 1:1-7.
- Du J, Dong L, Wang T, Yuan C, Fu R, Zhang L, Liu B, Zhang M, Yin Y, Qin J, Bouey J. Psychological symptoms among frontline healthcare workers during COVID-19 outbreak in Wuhan. General hospital psychiatry. 2020 Apr 3.
