Archive \ Volume.14 2023 Issue 1
Prevalence and Outcome of Management of Respiratory Distress Syndrome: A Systematic Review
Elham Ali Hammad Ali1*, Maha Ibrahim H Alanazi1, Ibrahim Awadh R Alanazi1, Basil Awadh Matar Alanazi2, Khaled Abdulaziz Alanazi1
1Department of Pediatrics, Maternity and Children Hospital, Arar, Saudi Arabia. 2Faculty of Medicine, Northern Border University, Arar, Saudi Arabia.
Abstract
The main goal of this review is about Respiratory distress syndrome, which starts within hours of delivery, is really a major cause of neonatal respiratory distress; it remains a leading cause of morbidity and mortality in preterm infants. The following search databases were used PubMed, the Web of Science, Science Direct, EBSCO, and the Cochrane Library. Utilizing Rayyan QCRI, studies papers were screened by title and abstract before being subjected to a full-text evaluation. This review investigates the published literature regarding the diagnosis and management of respiratory distress syndrome. A total of 314 studies were included for title screening. With outco2215 patients with respiratory distress syndrome, according to our study results, respiratory distress syndrome prevalence rates in Saudi Arabia ranged between 5.1% in Jeddah and the highest 84% in Al-Madinah. ARDS is still a leading cause of death and morbidity in children. Clinical outcomes can be improved by applying sound physiologic principles.
Keywords: Prevalence, Risk factors, Respiratory distress syndrome, Outcome of management, Saudi Arabia
INTRODUCTION
The newborn respiratory distress condition is a popular etiology of infant respiratory problems that manifest within a few hours after birth, most typically instantly following delivery. RDS mainly affects premature newborns, while mature infants are affected in rare instances. The prevalence of RDS is inversely proportionate to the newborn's stage of pregnancy, with younger and preterm newborns suffering from more severe illness. While prenatal corticosteroids, surfactants, and better newborn respiratory management may improve results for RDS infants, it remains a significant cause of morbidity and death in preterm babies [1].
Acute respiratory distress condition (ARDS) is a potentially fatal, acute, widespread inflammation form of lung damage associated with low oxygenation, respiratory infiltrates, and onset acuity. At the micro level, the condition is linked with vascular endothelium injury and widespread alveolar damage [2].
It is necessary to evaluate fetal Surfactant production and development of the lungs in order to comprehend the etiology of RDS. Normal fetal development of the lungs occurs in embryonic, pseudo-glandular, canalicular, saccular, and alveolar phases [3].
The term ARDS refers to a 7-day acute disease characterized by Infiltrates in both lungs and severe progressive hypoxia if no pulmonary edema is caused by cardiogenesis. The patient's ratio of arterial blood oxygen saturation (PaO2) to the oxygen percentage in inspired air defines ARDS (FiO2). The PaO2/FiO2 ratio in these patients is fewer than 300. In 2012, the ARDS definition was revised and became known as the Berlin definition. It varies from the prior definition by the European American Consensus in that it does not include the phrase "acute lung injury." It also eliminated the wedge pressure requirement 18 and added a requirement for PEEP (positive end-expiratory pressure) or CPAP (continuous positive airway pressure) 5 or more [4].
Patients with ARDS often have differing levels of pulmonary artery vascular constriction and might even eventually develop pulmonary hypertension. ARDS has a significant fatality rate, and there are limited effective therapeutic options available to address it [5].
ARDS was characterized by Matthay et al. 2019 as "adult-type respiratory distress" in a group of patients with increased respiratory failure, refractory hypoxemia, reduced functional reserve capacity, a decrease of lungs compliance, and diffused infiltrate on chest radiography [6-9]. In 1994, the American-European Consensus Conference (AECC) formally defined acute respiratory distress syndrome (ARDS) and acute lung injury (ALI). Acute hypoxemia, a PaO2 to FiO2 ratio of 300, bilateral infiltrates on chest radiography, less than 18 mmHg pulmonary artery wedge pressure, and the lack of left atrial hypertension characterize ALI. 5 ARDS is a severe type of ALI that has several of the same standards as ALI, with ARDS developing when the PaO2/FiO2 ratio is 200 [10].
Study Objective
The study aims to demonstrate the advantages, disadvantages, and risks of respiratory distress syndrome and a case study in the Kingdom of Saudi Arabia.
MATERIALS AND METHODS
In this systematic review, enhancing transparency in reporting the synthesis of qualitative research (ENTREQ) statement was used.
Study Design
A thorough evaluation of the available research on respiratory distress syndrome in Saudi Arabia is regarded as a reliable method of determining and synthesizing peer-reviewed publications in this field for evidence in order to develop a consistent empirical research program that builds on past knowledge. This review solely contained qualitative material to generate an interpretation. Furthermore, a qualitative data synthesis strives to provide findings that are meaningful, relevant, and suitable to individuals, to shape a research agenda, and, eventually, to more successfully impact Saudi Arabian policy and practices on respiratory distress syndrome. The material from the included studies was combined, integrated, and interpreted using qualitative synthesis approaches where possible.
The study attempts to go beyond data aggregation to give further interpretative perspectives on respiratory distress syndrome in Saudi Arabia and highlight where future research might contribute to what is known.
Criteria for Study Eligibility
The research comprised peer-reviewed qualitative research. Qualitative data from mixed methods research was assessed for inclusion and included if it was relevant. There were studies done in Saudi Arabia mentioned. All peer-reviewed studies published in English that reported on the prevalence and risk factors of respiratory distress syndrome from the perspective of the patient, family, healthcare worker, and healthcare delivery system were included. Only studies published between January 2012 and August 2021 were considered to ensure the work's currency while allowing a broad picture of developing difficulties to be recognized.
Study Participants
The review included all studies that report on respiratory distress syndrome from the perspective of children, families, and health workers that we came across in the studies on respiratory distress syndrome in Saudi Arabia.
Study Inclusion and Exclusion Criteria
The articles were chosen for their importance to the project, the English language, and geographical restrictions in Saudi Arabia. All other papers that did not have one of these subjects as their major goal, as well as repeated research and reviews, were eliminated. Any papers that were not available in English, conference abstracts, books or grey literature, and editorial comments were all eliminated by the reviewers. Studies that solely reported qualitative data were removed.
Search Strategy
To discover peer-reviewed literature on laser vaporization of oral lesions in Saudi Arabia, a systematic search method was created utilizing a mix of Medical Subject Headings (MeSH) and controlled vocabulary. The databases were PubMed/MEDLINE, Scopus/Embase (Elsevier), EbscoHost, and Google Scholar. The search was limited from January 2012 to August 2021.
Selection of Study
To show the selection methods and findings, the ENTREQ criteria [11] for reporting systematic qualitative reviews were employed. All retrieved studies were originally imported into the Endnote library to aid in removing duplication. Following the removal of duplicates, the Endnote library was shared by the two reviewers in order for them to separately screen the articles by title and abstract, guided by the eligibility criteria. The studies on which the two reviewers agreed were submitted to a full-text review. A third reviewer resolved any disagreements between the two reviewers. The whole text of all qualifying papers was independently reviewed by two reviewers. When there were disagreements between the two reviewers, a consensus was reached through discussion with the third reviewer. Finally, for the final framework synthesis, the entire texts of all relevant papers deemed to match the inclusion criteria were maintained.
Data Extraction
Data were independently extracted by two reviewers from research that are eligible onto a customized information extraction form filled up with variables pertaining to the investigation of populations and phenomena of interest. The third review author double-checked and verified the retrieved articles. The initial author's name and year of publication were retrieved, as well as the data collecting time and area in which the study was performed. Specific research information, such as study design, demographic, sample size, sampling techniques, and data-collecting procedures, are then recorded. The prevalence and risk factors for respiratory distress syndrome were thoroughly found in the Saudi population.
Data Synthesis and Analysis
The data were analyzed without the use of any program. The data was classified by theme by the reviewers, who then presented the themes in the form of an analysis table (chart). The table's columns and rows mirrored the research and associated topics, allowing us to compare study findings across different themes and subthemes.
Mapping and Interpretation
Charts were utilized by the reviewers to define the identified ideas and map the scope and character of the phenomena. To further understand the findings, the review investigated correlations between the concepts. The review was planned, and the findings were interpreted in accordance with the review objectives and emergent themes.
RESULTS AND DISCUSSION
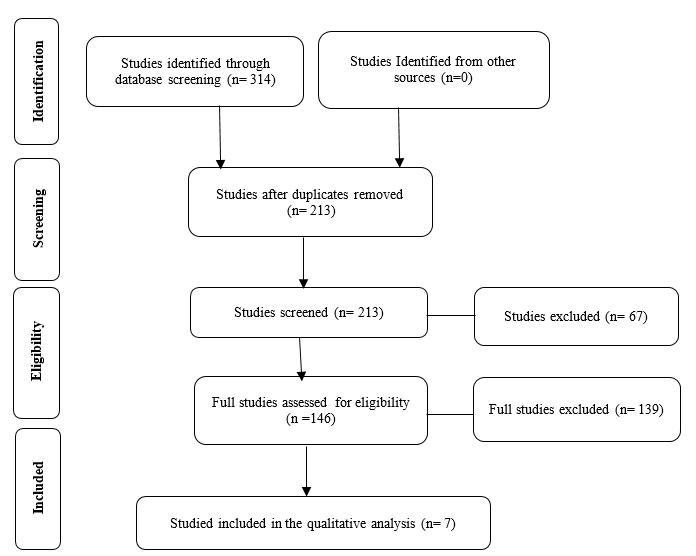
Figure 1 shows the selection and identification of studies. A total of 314 studies were included for title screening after a search of the aforementioned databases. Two hundred and thirteen of them were chosen for abstract screening, resulting in the removal of 67 papers. The remaining 146 full-text articles were examined. Due to differences in research aims, 139 papers were excluded from the full-text revision, and only seven were enrolled for final data extraction (Table 1).
According to our study results, respiratory distress syndrome prevalence rates in Saudi Arabia ranged between 5.1% in Jeddah and highest 84% in Al-Madinah [11, 12]. Saudi Arabia had a comparable prevalence of respiratory distress syndrome in several studies, 56%, 60%, 20% [13-15] also 8% of the cases admitted to the PICU unit.
Antibiotics were prescribed in 56.7% of cases; Amoxicillin was the first antibiotic prescribed in Ceftriaxone was used in 53.3% of instances, and it was used in 15.7% of cases, and Augmentin in 8.7% [16]. Hydroxychloroquine was the most commonly used medication in in the PICU. The COVID-19 regimen was followed with low molecular weight heparin and antiviral treatment [15].
|
|
|
Figure 1. Flow chart represents the data extraction process of the included studies |
|
Table 1. Author, country, year of publication, methodology, and outcome |
|||
|
Author, publishing year |
Region |
Participants |
Outcome |
|
Alfarwati et al. (2016) [11] |
Jeddah |
Fifty-nine term infants |
Fifty-nine term newborns with RDS (59/3601, 1.64%) were admitted to the NICU throughout the trial period, and 59 control infants were matched. Furthermore, RDS newborns had considerably lower birth weights and Apgar scores at one and five minutes. Although the RDS group had more cesarean sections and PROM, the difference was statistically insignificant. Three babies (5.1%) died in the RDS group. |
|
AlGhamdi et al. (2020) [13] |
Saudi Arabia |
Five hundred sixty-seven youngsters (51.5%) were males and (44.6%) ranged in age from 6 to 14 years. |
Asymptomatic patients accounted for 38.98% of the cases, with 319 (56%) suffering from mild illness and 27 (4.76%) suffering from the moderate-to-severe disease. Only ten (1.76%) patients needed to be admitted to the Pediatric Intensive Care Unit. The mortality rate, in this case, was determined to be 0.7%. After multivariate regression analysis, chronic lung diseases and low red blood cell count were determined to be significant predictors of moderate-to-severe illness. |
|
Alsahabi et al. (2019) [17] |
Riyadh |
A Saudi 4-month-old child with Down syndrome and an unrepaired atrioventricular septal defect (AVSD) |
The girl was hospitalized at Riyadh's first health cluster Al-Imam Abdulrahman Al Faisal Hospital. The medical care and clinical outcome of the baby are addressed. The infant was admitted after previously undergoing care at various facilities, and his health was worsening. The patient had acquired a rash and required oxygen therapy in addition to her regular prescription (furosemide and captopril). Ten days after her arrival, the patient's health improved and became clinically stable. She was released after two consecutive negative nasopharyngeal swabs. Based on the described instance, babies with DS and CHD should be considered high-risk COVID-19 patients and continuously followed. |
|
Alshengeti et al. (2020) [12] |
Al-Madinah |
Twenty-nine (27%) of the 106 patients had at least one pre-existing ailment, with bronchial asthma being the most prevalent (9.4%). In terms of COVID-19 disease severity, the majority of cases (84%), including one patient (0.94%), satisfied the MIS-C criteria. |
Patients were treated in accordance with Saudi Arabia's Ministry of Health guidelines. Nine (9.09%) patients needed pediatric ICU admission: five with severe or serious COVID-19 without antecedent conditions, one with MIS-C, two with metabolic problems, and one with chronic lung illness who was ventilator-dependent. On average, six patients (6.06%) required mechanical breathing for seven days. Antibiotics were given to 19 (19.1%) patients for suspected or confirmed secondary bacterial infection. However, only two (1.88%) positive bacterial cultures were recovered from endotracheal aspirates taken from two intubated patients within seven days of admission. |
|
AlMayouf et al. (2019) [18] |
Riyadh |
A total of 96 youngsters were hospitalized due to a confirmed COVID-19 infection, with 63.8% being under the age of three, 52.1% being boys, 96.9% being Saudi, 56.2% having an unidentified source of SARS CoV-2 infection, and 51% had no comorbidities. |
PICU care was necessary for ten (10.42%) of the 96 children hospitalized. The majority of them (60% required more than ten days in the hospital), yet the average PICU duration of stay was four days (70%). A small fraction of patients admitted to the PICU (20%) required intubation. Pneumonia (40%) and central nervous system problems (30%) were the most prevalent consequences. All patients received 100% oxygen, then 80% antibacterial antibiotics, and 40% steroids. The vast majority of patients (90%) fully healed and were released home (90%). We can confirm that one patient died in the intensive care unit. |
|
Albuali et al. (2020) [14] |
Saudi Arabia |
Three hundred ninety patients, the majority of participants, were from the Western area (247, or 63.3%), were female (203, or 52.1%), and were newborns (115, or 29.5%). |
The majority of patients were given supportive care. However, 14 patients were given hydroxychloroquine, five were given dexamethasone, and 20 were given a combination of medications. Complications were observed in 15 participants (3.85%), the majority of which were caused by secondary infection (60%). During the study period, only two patients died. The first case included a 1-year-old child with a neurological illness who had ARDS, while the second case involved a 10-year-old male who suffered shock despite having no comorbidities. |
|
Shaheen et al. (2018) [16] |
Makkah |
There were 908 prescriptions collected. Boys accounted for more than half of the cases (522/908), and girls accounted for 386/908 (42.5%). |
Antibiotics were provided in 515/908 instances (56.7%), either as a single therapy in 103/515 (20%), an antibiotic and antipyretic combination in 164/515 (31.8%), or antibiotics in combination with other medications in 248/515 (48.1%). Amoxicillin was administered as the initial antibiotic in 275/515 (53.3%) of cases, followed by Ceftriaxone in 81/515 (15.7%), Augmentin in 45/515 (8.7%), various other antibiotics in 90/515 (17.5%), and more than one antibiotic in 14/515 (2.7%). |
|
Kari et al. (2019) [15] |
Saudi Arabia |
There were 88 children enrolled (more than 20% of them were babies). Seven (8%) were in severe condition and needed to be admitted to the PICU. |
The most often utilized medicine in the COVID-19 regimen in the PICU was hydroxychloroquine, then low molecular weight heparin with antiviral therapy (lopinavir and ritonavir). However, these drugs were not routinely utilized in the general medical department. |
To understand the etiology of RDS, it is necessary to evaluate fetal lung development and surfactant production in order to comprehend the etiology of RDS. The embryonic, pseudo-glandular, canalicular, saccular, and alveolar phases of fetal lung development are all normal [19]. At 26 days, the lung bud emerges as a ventral projection of the fetal esophagus [20]. By 37 days, the mainstem bronchi have formed once the lung bud has penetrated and split across the surrounding mesenchyme. The mainstem bronchi have branched by 48 days, leading to the formation of subsegmental bronchi. The pulmonary vasculature had formed alongside the growing lung by 37 days, and the pulmonary artery had formed as a branch of the sixth aortic arch.
Neuroepithelial cells, cartilage, ciliated cells, goblet cells, and basal cells grow in the proximal pulmonary epithelium during the pseudo-glandular stage, which lasts from the fifth to the sixteenth week of pregnancy. The airways have branched 15 to 20 times by the 18th week of pregnancy [20].
The canalicular stage, which begins around the 16th week and ends around the 25th week, represents the start of the development of the pulmonary acinus, the establishment of a blood-air barrier, and surfactant synthesis via type 2 cells, resulting in a lung possibly viable for gas exchange. The mesenchyme is being vascularized by increasing numbers and sizes of capillaries. The mesenchymal gap between the respiratory epithelial basement membranes and the vascular epithelium narrows due to this and bronchiole development. These basement membranes of capillaries and respiratory epithelial cells eventually fuse to form a rudimentary blood-air barrier [21]. Lamellar bodies begin to develop in the cytoplasm of the glycogen-laden cuboidal epithelium of the bronchiole at 20 weeks, and these cells convert into type 2 cells capable of generating surfactant.
Acute respiratory distress syndrome (ARDS) is one of the most common reasons for ICU admission [7, 22]. Children are also affected by non-cardiogenic pulmonary edema and hypoxia syndrome, which is associated with significant mortality in pediatric intensive care units (PICU). Diagnosis of child ARDS is based on the presence of hypoxia and a new chest infiltration within seven days after a known insult (PARDS). ARDS is distinguished by hypoxemia, which is accompanied by reduced lung compliance, increased labor of breathing, and poor gas exchange. Death is typically accompanied by multiple organ dysfunction or failure. As in adults, supportive therapy and lung-protective ventilator support remain the basis of the treatment in children. The illness entity is currently unknown to non-ICU pediatric healthcare personnel [23].
The major histologic alterations in ARDS demonstrate the existence of alveolar edema in sick lung regions. Moreover, proteinaceous fluid and blood flow into the alveolar airspace due to type I pneumocytes and vascular endothelium damage. Alveolar hemorrhage, pulmonary capillary congestion, interstitial edema, and the creation of a hyaline membrane are all possible signs. None of these modifications are disease-specific [24].
Unfortunately, no medicine has been proven to be beneficial in preventing or treating ARDS. The primary treatment technique is supportive care, which aims to 1) reduce the shunt fraction, 2) increase oxygen supply, 3) reduce oxygen use, and 4) avoid future harm. Until they improve, patients are mechanically ventilated, given diuretics to prevent fluid excess, and nutritional care. Surprisingly, the style of ventilation of a patient affects lung healing. According to data, several ventilatory methods may worsen alveolar damage and prolong lung injury in the context of ARDS. Preventing volutrauma (exposed to large tidal volumes), barotrauma (exposed to high plateau pressures), and atelectrauma (exposed to atelectasis) is a priority [25, 26].
CONCLUSION
ARDS is still a leading cause of death and morbidity in children. Clinical outcomes can be improved by applying sound physiologic principles.
Even those that survive may have to make do with a lesser living level. While there are multiple risk factors for ARDS, there is no way to avoid the syndrome. In addition to hydration restriction in high-risk individuals. The team must keep a close eye out for hypoxia. The sooner hypoxia is detected, the better the outcome. Hence, those who survive must undergo intensive therapy to restore their functional condition. Many persons have dyspnea even after light exercise and must rely on others for assistance.
ACKNOWLEDGMENTS: Many thanks to Dr. Elham Ali Hammad Ali; Pediatric Consultant, Maternity and children hospital in Arar, Saudi Arabia, for her continuous help, support and encouragement to complete this work.
CONFLICT OF INTEREST: None
FINANCIAL SUPPORT: None
ETHICS STATEMENT: None