Archive \ Volume.11 2020 Issue 1
Characteristics of Children with Alagille Syndrome at Children’s Hospital No. 1, Vietnam
Tram Van Ta 1*, Truong Viet Nguyen 2, Hien The Pham 3, Tuan Anh Nguyen 2
1 Tien Giang General Hospital, Tien Giang province, Vietnam. 2 Children Hospital No.1 in Ho Chi Minh City, Ho Chi Minh City, Vietnam.
3 Le Loi Hospital, Ba Ria - Vung Tau province, Vietnam.

Abstract
Background: Alagille syndrome (ALGS) is an autosomal dominant disorder that can affect the liver, heart, eyes, vertebrae, and face. ALGS is caused by mutations in the Notch signaling pathway members JAG1 or NOTCH2. The estimated prevalence of ALGS is 1 in 70,000 newborns. JAG1 gene mutations cause more than 90 percent of ALGS cases. This study aimed to determine the clinical, subclinical, and genetic mutation characteristics of ALGS in children in Vietnam. Materials and Methods: This cross-sectional study was conducted on all ALGS children treated in the Gastroenterology Department at Children’s Hospital No. 1 from September 2014 to September 2017. Results: Of the 30 enrolled ALGS cases, most patients that came from other provinces, were admitted to hospital mainly due to jaundice, and showed no significant differences in age or sex. The clinical features included 96.67% hepatic abnormalities, 80% spinal abnormalities, and 86.67% characteristic ALGS facial features. Subclinical features included significant increases in direct bilirubin and gamma-glutamyl transferase (GGT) levels. JAG1 mutations were found in 73.33% of the cases and included missense (32%), nonsense (36%), frameshift (23%), and splice site (9%) mutations. The most frequent mutation position was exon 4 (23.33%), with the remainder located throughout the JAG1 gene. Conclusion: Children with ALGS most frequently showed hepatic abnormalities, skeletal abnormalities, and characteristic facial features. Direct bilirubin and GGT indexes were strongly increased in all cases. JAG1 mutation was the main cause of ALGS. ALGS is novel in Vietnam, so more research is needed.
Keywords: Alagille syndrome, children, JAG1 mutation, hepatic disease, cardiac disease.

INTRODUCTION
Alagille syndrome (ALGS) is an autosomal dominant disorder that mainly affects the liver, heart, eyes, spinal column, and face.[1] The disease occurs due to mutations in either the Jagged1 (JAG1) or NOTCH2 genes of the Notch signaling pathway. The diagnosis of ALGS is based on the presence of a mutant gene plus a major clinical symptom. Treatment is mainly uplifting and proper nutrition. The prognosis is mainly based on the pathology of the liver and heart.
Many research studies have been conducted globally on the clinical characteristics of ALGS. The results from genetic studies have also helped in the detection of more than 90% of the different genetic mutations in ALGS clinical diagnosis cases. [2-4] However, if based solely on clinical manifestations, ALGS is often easily misdiagnosed as other conditions, especially biliary atrophy in infancy. This leads to children undergoing inappropriate interventions that affect the prognosis of the disease.
We have not found any published research on ALGS in Vietnam. The aim of this study was therefore to describe the clinical and subclinical characteristics and genetic mutations in Vietnamese children with ALGS, to contribute to an early and definitive diagnosis, as well as to identify the typical genetic mutations characteristics of children with ALGS in Vietnam.
MATERIALS AND METHODS
A cross-sectional descriptive study was conducted with pediatric patients clinically diagnosed with ALGS and being treated at the Department of Gastroenterology at Children’s Hospital No.1, Ho Chi Minh City, Vietnam, from September 2014 to September 2017. Children 15 years of age or younger with three or more clinical symptoms were selected for the study. The clinical symptoms included hepatic abnormalities, cardiac abnormalities, eye abnormalities, spinal abnormalities, and characteristic ALGS facial features. Children diagnosed with other causes, such as extrahepatic biliary atrophy, or whose direct guardian declined participation were excluded from the study.
The selected children admitted to the Gastroenterology Department with signs suspicious for ALGS underwent a specialist examination and tests. Children with 3 or more clinical symptoms underwent further study, including genetic testing for JAG1 and NOTCH2 mutations.
Statistical Analysis
Data were entered using Epidata 3.1 and analyzed using Stata 13. Descriptive statistics were expressed as frequency and percentage for qualitative variables. Quantitative variables that did not have normal distributions were described by medians and quartiles.
Ethical Considerations
This study was approved by the Scientific Research Committee of Children’s Hospital No. 1. The collected data were only used for this study and not for any other purpose. Participation was voluntary and anonymous. The children's guardians were asked to sign informed consent forms before enrollment.
RESULTS
Characteristics of Patients
In total, 30 children with a median age of 8 months were included in the study. No significant differences were noted for their age or gender. The majority of the children (76.67%) came from provinces outside Ho Chi Minh City. The main reason for hospitalization was yellow skin (63.33%), and most children (56.67%) had four clinical symptoms.
|
Table 1: Demographic and medical characteristics of patients (N=30) |
||
|
Characteristics* |
|
|
|
Age, months (median, quartiles) |
8 (2 : 54) |
|
|
Age group |
≤ 1 year old |
14 (46.67) |
|
|
> 1 year old |
16 (53.33) |
|
Gender |
Female |
13 (43.33) |
|
|
Male |
17 (56.67) |
|
Place to live |
Ho Chi Minh City |
7 (23.33) |
|
|
Other provinces |
23 (76.67) |
|
Reason for admission |
Yellow skin |
19 (63.33) |
|
|
Pruritus |
4 (13.33) |
|
|
Ascites |
4 (13.33) |
|
|
Others |
3 (0.1) |
|
Number of symptoms |
3 |
7 (23.33) |
|
|
4 |
17 (56.67) |
|
|
5 |
6 (20) |
|
*Exempt age, values are the number (percentage) of patients with the characteristic |
||
Clinical Characteristics of ALGS Children
Most children had hepatic abnormalities, spinal abnormalities, and typical facial characteristics associated with ALGS (≥ 80%). Cardiac abnormalities accounted for 76.67% of the cases, and eye abnormalities were the least frequent (43.44%). Only one case showed renal abnormalities.
|
Table 2: Clinical characteristics of patients (N=30) |
||
|
Clinical characteristics |
N (%) |
|
|
Hepatic abnormalities |
No |
1 (3.33) |
|
|
Yes |
29 (96.67) |
|
Cardiac abnormalities |
No |
7 (23.33) |
|
|
Yes |
23 (76.67) |
|
Spinal abnormalities |
No |
6 (20) |
|
|
Yes |
24 (80) |
|
Eye abnormalities |
No |
13 (43.33) |
|
|
Yes |
17 (56.67) |
|
Characteristic facial features |
No |
4 (13.33) |
|
|
Yes |
26 (86.67) |
|
Renal abnormalities |
No |
29 (96.67) |
|
|
Yes |
1 (3.33) |
The majority of children showed chronic cholestasis (96.67%) and 30% of the children had hepatomegaly. Ultrasound of the abdomen showed that the main abnormalities were hepatomegaly/splenomegaly. One case had bilateral renal dysplasia and another had hepatic hemangioma. Liver biopsies of nine cases showed biliary atresia.
|
Table 3: Manifestations of hepatic abnormalities (N=30) |
||
|
Manifestations |
N (%) |
|
|
Chronic intrahepatic cholestasic |
No |
1 (3.33) |
|
|
Yes |
29 (96.67) |
|
Hepatomegaly |
No |
21 (70) |
|
|
Yes |
9 (30) |
|
Abdominal ultrasound |
Normal |
10 (33.33) |
|
|
Hepatomegaly/splenomegaly |
10 (33.33) |
|
|
Small gallbladder |
3 (10) |
|
|
Cirrhosis |
5 (16.67) |
|
|
Other abnormalities |
2 (6.67) |
|
Liver biopsy (n=9) |
Biliary atresia |
9 (30) |
Heart murmurs were found in 66.67% of the children. Abnormalities on echocardiography were primarily pulmonary artery abnormalities, with one case of tetralogy of Fallot. An opaque ring behind the cornea was present in 17 cases, and 24 children had butterfly-shaped vertebrae
|
Table 4: Manifestations of cardiac abnormalities (N=30) |
||
|
Manifestations |
N (%) |
|
|
Heart murmur |
No |
10 (33.33) |
|
Yes |
20 (66.67) |
|
|
Echocardiography |
Pulmonary artery stenosis (left) |
2 (8.7) |
|
|
Pulmonary artery stenosis (right) |
1 (4.35) |
|
|
Pulmonary artery stenosis (right and left) |
4 (17.39) |
|
|
Pulmonary valve stenosis |
1 (4.35) |
|
|
Pulmonary stenosis and other |
14 (60.87) |
|
|
Other abnormalities |
1 (4.35) |
|
Table 5 Manifestations of an eye and spinal abnormalities (N=30) |
||
|
Manifestations |
N (%) |
|
|
Eye abnormalities |
No |
13 (43.33) |
|
|
Opaque ring behind cornea |
17 (56.67) |
|
Spinal abnormalities |
No |
6 (20) |
|
|
Butterfly shape of vertebrae |
24 (80) |
Subclinical Characteristics of Children with ALGS
The subclinical indices were higher than normal in the children with ALGS. The median values for gamma-glutamyl transferase (GGT) and the direct bilirubin index (bilirubin TT) were 21.4-fold and 23.21-fold higher, respectively, when compared to normal values.
|
Table 6: Laboratory testing (N=30) |
||
|
Laboratory testing |
Median (quartiles) |
Comparison with normal (times) |
|
Bilirubin TP (µmol/L) |
146.97 (59.3:206.2) |
7.16 |
|
Bilirubin TT (µmol/L) |
79.4 (32.6:108.5) |
23.21 |
|
SGOT (U/L) |
212.67 (174.9:306.1) |
3.54 |
|
SGPT (U/L) |
197.6 (97.6:302) |
4.39 |
|
ALP (U/L) |
476.4 (393.6:759) |
1.38 |
|
GGT (U/L) |
470.9 (230:1094.5) |
21.4 |
|
Cholesterol (mmol/L) |
6.2 (5.31:10.9) |
1.18 |
|
Triglycerid (mmol/L) |
2.5 (2.1:3.9) |
1.45 |
Genetic characteristics of children with ALGS
A JAG1 mutation was found in 73.33% of the children with ALGS. The major mutation types were nonsense (36%) and missense (32%). Splicing mutations had the lowest rate (9%). The most common mutations were in the exons of the JAG1 gene, with exon 4 mutations being the most common (7 cases).
|
Table 7: Mutation rate (N=30) |
||
|
|
N (%) |
|
|
JAG1 mutation |
No |
22 (73.33) |
|
|
Yes |
8 (26.67) |
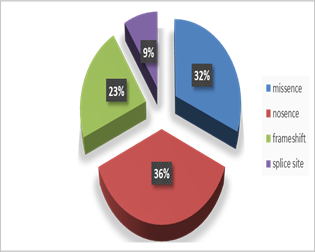
Figure 1: Types of mutations (N=22)
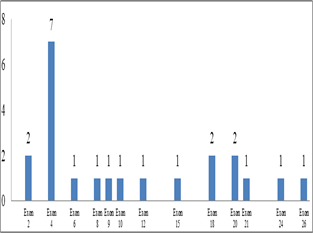
Figure 2: Mutation positions (N=22)
DISCUSSION
The most common clinical characteristics of ALGS in the Vietnamese children in the present study group were hepatic (96.67%) and facial (86.67%) abnormalities. This finding is similar to the findings of Cho et al.. [2] in Korea, who reported hepatic abnormalities in 89% and facial abnormalities in 100% of their cases. Emerick et al. [3] reported ratios similar ratios of 85% and 96%, respectively, as did Alagille et al.,[1] at 91% and 95%.
Our research also revealed spinal abnormalities (80%) at rates similar to those reported by Alagille et al. [1] at 87%, but these rates were higher than those of Cho et al. [2] and Emerick et al. [3] at 47% and 51%, respectively. Cardiac abnormalities (76.67%) were lower than those reported previously, at 95%,[2] 97%, [3] and87%.[1] The results for eye abnormalities (56.67%) were similar to those reported by Cho et al., [2] but were much lower than those of Emerick et al. [3] (78%) and Alagille et al. [1] (88 %). Conversely, the occurrence of renal abnormalities was much less frequent than reported by Emerick et al. [3] (40%). These differences in the occurrence of abnormalities may reflect differences in sample sizes, subjects, and locations.
Nearly all the children with hepatic abnormalities expressed chronic cholestasis. About one-third of the children had hepatomegaly detected with physical examination and abdominal ultrasound. The abdominal ultrasound results also indicated the presence of biliary atresia and signs of cirrhosis. Two cases, in particular, had bilateral renal dysplasia and hemangioma. Liver biopsy of nine cases of ALGS confirmed biliary atresia. Hepatic disease in ALGS manifested with a wide range of clinical severity, even in patients with the same genetic mutation. The classic finding on liver biopsy was bile duct paucity; however, this was not diagnostic and not all children with Alagille syndrome show this paucity in liver biopsies. [5]
During the clinical examinations, we recorded 20 cases with a heart murmur. All 30 cases underwent echocardiography and 23 had abnormal results. The major abnormality was a pulmonary artery abnormality, including an isolated narrow left or right branch, (or both branches), pulmonary valve stenosis, or pulmonary stenosis associated with other abnormalities (e.g., ventricular septal defect, atrial septal defect, aortic stenosis, mitral stenosis or 2-leaf or 3-leaf valves). One case of tetralogy of Fallot was diagnosed. This result was much lower than that reported by Emerick et al. [3] at 11%. Our results showed that pulmonary artery abnormalities were often combined with other abnormalities (60.87%). Conversely, Emerick et al. [3] found the common abnormalities to be primarily peripheral pulmonary stenosis (67%). This difference may again reflect differences in sample size.
Similar to the findings of previous studies, the common eye abnormalities in our study were an opaque ring behind the cornea. The common spinal abnormalities were a butterfly-shaped vertebra on a straight X-ray of the spine.
Research results on subclinical indicators in the ALGS cases showed whole serum bilirubin (bilirubin TP), bilirubin TT, aspartate aminotransferase (SGOT), alanine transaminase (SGPT), alkaline phosphatase (ALP), and GGT, cholesterol, and triglyceride levels above the normal values. In particular, the bilirubin TT and GGT showed very high increases. These findings were consistent with the chronic cholestasis of children with ALGS.
The genetic characteristics of the children with ALGS children indicated that 73.33% had a JAG1 mutation. This ratio was similar to previously published values.[2, 4, 6–8] The characteristics of the JAG1 mutation included missense, nonsense, frame shift, and splice-site mutations, in agreement with previous research. However, the most common mutation reported in previous studies the frame shift type, whereas the most common mutations in our study were nonsense mutations (36%).
|
Table 8: Statistics of mutation types from other studies |
||||
|
|
Mutant types |
|||
|
Missense |
Nonsense |
Frame shift |
Splice site |
|
|
Cho JM (2014) |
3 (21.4%) |
3 (21.4%) |
0 |
8 (57.2%) |
|
Crosnier C (1999) |
13(18.8%) |
14 (20.3%) |
11 (16%) |
31 (44.9%) |
|
Jurkiewicz D (2014) |
4 (15.4%) |
5 (19.2%) |
2 (7.7%) |
7 (26.9%) |
|
Krantz ID (1998) |
2 (6%) |
9 (26%) |
4 (11.4%) |
20 (57%) |
|
Li L (2015) |
6 (9.4%) |
16 (22.9%) |
8 (11.4%) |
35 (50%) |
We also did not detect any cases with deletion mutations, although these mutations accounted for 30.7% of the mutations found by Jurkiewicz et al. [8] and 7.1% of the mutations reported by Li et al. [4] This difference may reflect differences in sample size or mutant analysis techniques. The mutant types were mostly distributed in the JAG1 gene exons, and particularly in exon 4, in agreement with previous research.
CONCLUSION
A study of 30 children with ALGS at The Children Hospital No. 1 from September 2014 to September 2017 showed no significant difference in age group or gender. Patients from other provinces (outside Ho Chi Minh City) were the majority and patients were hospitalized mostly for yellow skin.
The most common abnormalities were in the liver, spine, and face. Cardiac abnormalities were less common and were mainly associated with pulmonary stenosis. The occurrence of eye abnormalities was very low. Regarding subclinical characteristics, the indicators of bilirubin TT and GGT showed very high increases. A JAG1 gene mutation was detected in most cases of ALGS and was most frequently a nonsense mutation. Mutations appeared on mostly JAG1 exons but were most frequent on exon 4.
REFERENCES
- Alagille, D., A. Estrada, M. Hadchouel, M. Gautler, M. Odievre, and J. P. Dommergues. "Syndromic paucity of interlobular bile ducts (Alagille syndrome or arteriohepatic dysplasia): review of 80 cases." The Journal of pediatrics, 1987; 110(2): 195-200.
- Cho, Jin Min, Seak Hee Oh, Hyun Jin Kim, Joon Sung Kim, Kyung Mo Kim, Gu‐Hwan Kim, Eunsil Yu, Beom Hee Lee, and Han‐Wook Yoo. "Clinical features, outcomes, and genetic analysis in Korean children with Alagille syndrome." Pediatrics International, 2015; 57(4): 552-557.
- Emerick, Karan M., Elizabeth B. Rand, Elizabeth Goldmuntz, Ian D. Krantz, Nancy B. Spinner, and David A. Piccoli. "Features of Alagille syndrome in 92 patients: frequency and relation to prognosis." Hepatology, 1999; 29(3): 822-829.
- Li, Liting, Jibin Dong, Xiaohong Wang, Hongmei Guo, Huijun Wang, Jing Zhao, Yiling Qiu, Kuerbanjiang Abuduxikuer, and Jianshe Wang. "JAG1 mutation spectrum and origin in Chinese children with clinical features of Alagille syndrome." PloS one, 2015; 10(6).
- Kriegermeier A, Wehrman A, Kamath BM, Loomes KM. Liver disease in alagille syndrome. In Alagille syndrome: Pathogenesis and clinical management, B. M. Kamath, and K. M. Loomes (eds.). Springer International Publishing, New York, 2018, 49–6
- Crosnier, Cécile, Catherine Driancourt, Nicole Raynaud, Sophie Dhorne–Pollet, Nicolas Pollet, Olivier Bernard, Michelle Hadchouel, and Michèle Meunier–Rotival. "Mutations in JAGGED1 gene are predominantly sporadic in Alagille syndrome." Gastroenterology, 1999; 116(5): 1141-1148.
- Krantz, Ian D., Raymond P. Colliton, Anna Genin, Elizabeth B. Rand, Linheng Li, David A. Piccoli, and Nancy B. Spinner. "Spectrum and frequency of jagged1 (JAG1) mutations in Alagille syndrome patients and their families." The American Journal of Human Genetics, 1998: 62(6): 1361-1369.
- Jurkiewicz, Dorota, Dorota Gliwicz, Elżbieta Ciara, Jennifer Gerfen, Magdalena Pelc, Dorota Piekutowska-Abramczuk, Monika Kugaudo, Krystyna Chrzanowska, Nancy B. Spinner, and Małgorzata Krajewska-Walasek. "Spectrum of JAG1 gene mutations in Polish patients with Alagille syndrome." Journal of applied genetics, 2014; 55(3): 329-336.
