Archive \ Volume.15 2024 Issue 2
Drug Utilization Analysis of Analgesics and Adjuvants Used in Pain Management
Abstract
Pain is a multidimensional sensation that arises from a physiologic and psychological response to an unpleasant experience. Pain is an alarm signal that causes an organism to pull away from potentially harmful stimuli, thereby protecting itself from potential damage. In most cases, it is associated with an injury or the possibility of an injury. Here we develop and carry out drug utilization evaluations concerning the analgesics and adjuvants in pain management. The analgesics and adjuvants were further classified to include in the program standards and criteria for the selected drugs and compared with the actual drug utilization. Cross-sectional, observational case study with 377 patients. Patients aged > 18 years and < 80 years experiencing pain were included in the study. Age < 18 years, > 80 years. Pregnant or lactating women were excluded from the study. Out of the total drugs (1362), total antibiotics prescribed were about 45 (3.30%). Among them, 35(2.6%) were prescribed in tablet form, (0.44%) were prescribed in injection form either i.v or i.m, 3(0.22%) were prescribed in powder form (gastolac sachets), 1 (0.07%) was prescribed in ointment form. Cefuroxime + clavulanic acid prescribed was the most commonly used 13 (0.95%). This study reveals a pattern of analgesic use that includes the administration of extensive oral analgesic preparations, a high generic naming of medications, and the appropriate use of these pharmaceuticals concerning the dosage strength, the frequency of treatment, and the duration of therapy.
How to cite:
Download Citation
INTRODUCTION
Pain is a complex perception that arises from a combination of physiological and psychological responses to a noxious stimulus [1]. Pain is an alarm mechanism that prompts an organism to retreat from hazardous stimuli, safeguarding it from potential harm [2]. Commonly, it is associated with physical harm or the likelihood of physical harm. The subjective nature of pain, which encompasses both emotive and sensory aspects, renders its definition a challenging task.
The development of individual pain responses is shaped during childhood and is subject to various factors, such as social, cultural, psychological, cognitive, and genetic factors. The neuroanatomical foundation for pain reception is also established prenatally [3]. These factors elucidate the reasons behind the variability in individuals' pain tolerance. One of the primary functions of pain is to alert the body of impending danger. Nociception, which refers to the neural processing of painful stimuli within the brain, facilitates this phenomenon. The nociceptive response encompasses a range of physiological reactions beyond pain perception, such as heightened blood pressure, elevated heart rate, and an automatic withdrawal from the noxious stimuli, including more than just the pain feeling [4].
The fracture of a bone or exposure to a high-temperature surface can trigger the experience of acute pain. Acute pain is a sudden, severe, and transitory sensation often likened to a piercing, sharp feeling [5]. Subsequently, a persistent sensation of dull throbbing ensues. Chronic pain poses greater difficulty in identification and presents a heightened risk due to its frequent association with ailments such as cancer or arthritis. The exacerbation of pain may occur in cases where psychological conditions such as melancholy and anxiety are not effectively alleviated [6]. A distressing sensory and emotional experience associated with, or resembles actual or potential damage to bodily tissues [7].
Pain has rendered 50 million Americans either wholly or partially incapacitated. It is possible to estimate that the annual cost of suffering to US society is billions of dollars. At some point in their lives, an estimated 25 million Americans will suffer from severe chronic pain [8]. As more Americans labor past 60 and live into their 80s, these figures are predicted to grow.
Unfortunately, inpatient and long-term care facilities and the general public frequently undertreat pain [9]. Hospitalized patients who were ill reported a 50% pain incidence; 15% of these patients experienced extremely or moderately severe pain at least 50% of the time, and 15% were unsatisfied with overall pain management. In the Michigan pain research, 22% of chronic pain patients thought treatment made their pain worse, and 70% said that they continued to experience pain after receiving treatment [10, 11].
The evidence of previous research shows that very few studies were conducted in Indian hospital settings about analgesics and adjuvants use in pain management. Because of the high impact of analgesics and adjuvant drug use on patient’s health, there was a high need to address the use of drugs in pain management. This drives us to the need to plan the Drug Utilisation Analysis (DUA) study on analgesics and adjuvants in pain management to develop and carry out drug utilization assessments pertaining to the analgesics and adjuvants used in pain management. This research's specific objectives are to identify analgesics and adjuvants and classify them in the pain management program. To develop the standards and criteria for the selected drugs and compare them with the actual drug utilization. To identify and rectify drug-related problems in pain management and provide feedback to Health Care Professionals (HCP). Also, to highlight the application of DUA indicators.
MATERIALS AND METHODS
Place of Study
"A Study on Drug Utilization Evaluation of Analgesics and Adjuvants Used for the Management of Pain" was conducted at GK Speciality Hospital, adjacent to Ravi Pediatric Hospital in Kasthuridevi Nagar, Pogathota, Nellore, and Andhra Pradesh.
Study Duration
The study lasts six months (December 2021 to May 2022).
Type of Study
A case study with a cross-sectional, observational design.
Cross-sectional investigations are observational and are referred to as descriptive research, not causal or rational, so you cannot use them to determine the cause of the disease [12]. Researchers document the population's information, but they do not manipulate variables. This type of research can describe community characteristics but not establish cause-and-effect relationships between various variables.
Sample Size
n = 377 patients.
The total number of patients enrolled in the research investigation was 402. Of these, 25 patients did not fulfill the eligibility criteria and were excluded from the analysis.
Study Materials
Patient Informed Consent Form (PICF)
A specially designed Patient Data Collection Proforma (PDCP)
Study Criteria/Patient Enrolments
Participants were recruited in the study based on the inclusion and exclusion criteria that have been established.
Inclusion Criteria
- Patients aged > 18 years and < 80 years experiencing pain.
- All male and female patients except pregnant and lactating women.
Exclusion Criteria
The following requirements were disregarded throughout the process of the investigation:
- Participants under the age of 18 or over the age of 80;
- Women who were pregnant or nursing;
- Participants with a history of gastrointestinal, renal, or liver disease; and participants with any history of psychiatric illness.
Data Collection Methods
A standardized data entry method was used to collect data from the hospital.
To determine the extent of the investigation, a pilot study was conducted for two weeks in the hospital [13-16]. All analgesic and adjuvant prescriptions were tracked to determine the dosage, dosage form, route of administration, extent of analgesic use, and the conditions for which they were prescribed. Literature was gathered and reviewed for the study on the significance of corticosteroid prescribing patterns in dermatology.
Obtaining Consent from the Hospital Authority
The hospital's Department of pharmacy practice conducted the study following the previous reports [17-21]. The institutional ethics committee approved the study protocol detailing the planned title, study location, inclusion and exclusion criteria, objective, and work methodology. Written permission to conduct the study was obtained from the hospital's resources and the doctors in charge of the different departments. At the same time, informed patient consent was obtained from all participants.
Collection of Data
The trial enrolled 402 patients in total. To improve the accuracy of the parameters, 25 of these patients were eliminated from the study since they did not meet the eligibility requirements. Prescriptions from patients were gathered. A total of 377 doctor-written prescriptions were gathered at random and examined.
Analysis of Data
Following careful consideration of the inclusion and exclusion criteria, the prescriptions of the chosen patients were gathered, and they were assessed for the completion of the following variables: Patient personal information: Age, and sex. Reason for the hospital visit, prescribed medications, administration method, and adverse drug interactions.
Evaluation of Data
The information about the use of analgesics and adjuvants in the prescription and a summary of pain management techniques were used to assess the data gathered from all of the prescriptions.
Analysis of Statistics
Descriptive statistics were used to analyze the data, and Microsoft Excel frequency distribution tables were used to display the findings. Age demographic information was expressed as an average mean, while gender information was expressed as a percentage.
Ethics Approval
The study was approved by the Institutional Ethics Committee of A C Subba Reddy Government Medical College & Hospital Dargamitta, Nellore 524004 Andhra Pradesh, India with a reference number Regd No: ECR/961/Inst/AP/2017/RR-20.
RESULTS AND DISCUSSION
Between December 2021 and May 2022, 402 patients were included in the study across six months. Three hundred seventy-seven patients were analyzed after 25 of these patients were removed from the analysis because they did not meet the eligibility requirements. Thus, the current study was conducted on 377 patients who were receiving medical care at GK Speciality Hospital, located at 16/1196, Kasturidevi Nagar, Pogathota, Nellore, and Andhra Pradesh.
Disease Pattern among Study Subjects Receiving Analgesics
In our study, the clinical indications for prescribing analgesics in this hospital for pain arelower back pain was found to be the major clinical complaint of the patients - 73(19.3%); followed by trauma and post operative cases - 61(16.2%); osteoarthritis knee - 58(15.4%); other pains such as foot pain, hip pain, neck pain, hand pain, shoulder pain, head ache, leg pain, proximal tibia pain, wrist pain, epigastric pain, calf pain, ankle pain, knee pain and 1/3rd tibia pain - 47(12.5%); CBN (Cervicobrachial neuralgia) - 19(5%); PA shoulder (Per arthritis shoulder also called Frozen shoulder) - 16(4.2%); arthritis such as rheumatoid arthritis, polyarthritis, septic arthritis - 13(3.4%); cellulitis - 11(2.9%); pains such as myalgias, fibromyalgia and post viral arthralgia - 10 (2.7%); synovitis - 7(1.9%); RCT (Rotatory cuff tear) - 6(1.6%); spondylosis - 6(1.6%); plantar fasciitis - 5(1.3%); De Queveris tenosynovitis - 4(1.06%); coccydynia - 4(1.06%); spondylolysthesis grade Ⅰ & Ⅱ - 4(1.06%); LCS (Lumbar canal stenosis) - 4(1.06%); tennis elbow - 3(0.8%); hematoma, hematoma with abscess, lymphadenopathy - 3(0.8); lumbar scoliois - 3(0.8%); AVN (avascular necrosis) - 2(0.5%); PIVD (Prolapsed Intervertebral Disc) - 2(0.5%); trigger finger - 2(0.5%); trigger thumbs - 2(0.5%); osteoporosis - 2(0.5%); Pott’s spine - 2(0.5%); infrapatellar bursitis - 1(0.3%); RCB (retrocalcaneal bursitis) - 1(0.3%); Ganglion - 1(0.3%); Saturday wrist palsy - 1(0.3%); IDK of left knee 1(0.3%); meralgiaparasthesias - 1(0.3%); bilateral genuvalgum knee - 1(0.3%); carpal tunnel syndrome - 1(0.3%).
Demographics
Age Distribution
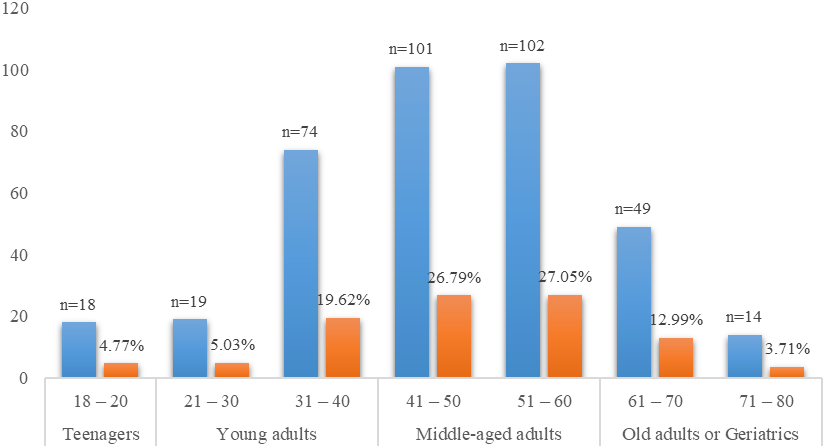
According to our research, the overall sample size's average age is 53.85 (plus or minus 15.60). Out of 377 patients, 27.5% were from the 51- to 60-year-old age range, followed by 26.79% from the 41- to 50-year-old middle-aged adult range, 19.62% from the 31- to 40-year-old young adult range, 12.99% from the 61- to 70-year-old old adult range, 5.03% from the 21- to 30-year-old young adult range, and 4.77% and 3.71% from the 18- to 20-year-old teenager Figure 1. On the other hand, the gender distribution out of the 377 patients that comprised the study's participant population, 154 (40.8%) were men and 223 (59.2%) were women. It shows that in comparison to male patients, female patients were found to be relatively more numerous.
|
|
|
Figure 1. Age distribution of the study population |
The Pattern of Analgesics Prescribed for the Study Population
The Pattern of Analgesics Prescribed for Oral Route of Administration (Tablets)
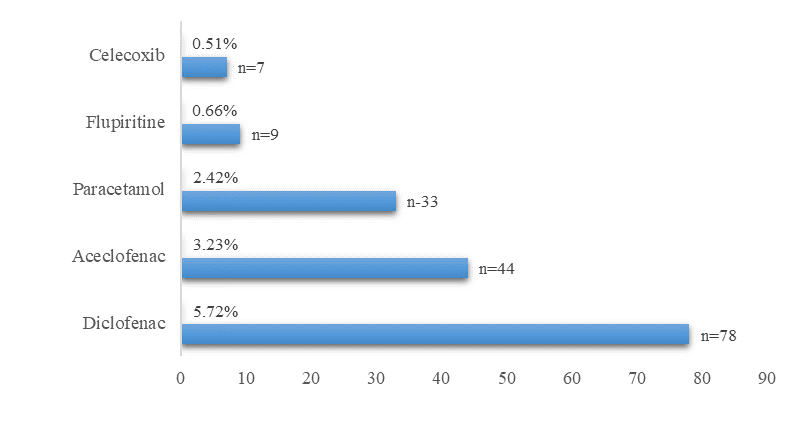
In our study, out of 377 cases, (552) 40.5% analgesics were prescribed out of 1,362 drugs. Out of 40.5%, tablets prescribed were 423 (31.05%). Monotherapy prescribed was 171 (12.6%). Diclofenac prescribed were78 (5.72%), followed by aceclofenac prescribed 44 (3.23%), paracetamol prescribed 33 (2.42%), fluperitine prescribed 9 (0.66%), and celecoxib prescribed was 7 (0.51%) Figure 2.
|
|
|
Figure 2. Distribution of monotherapy drugs |
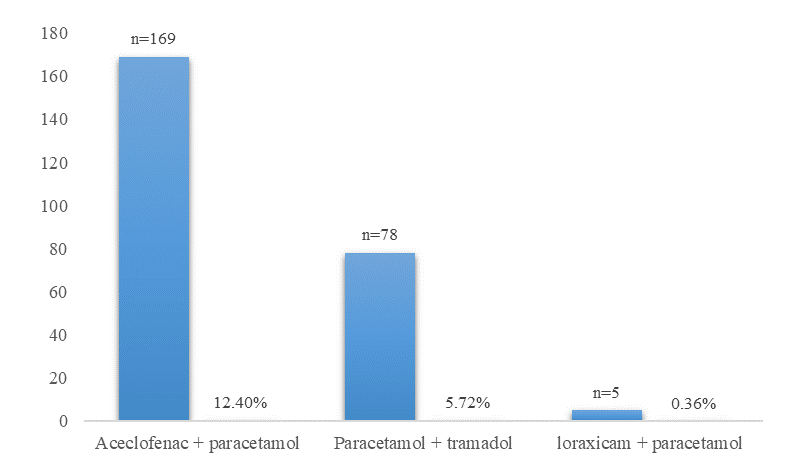
Combinational therapy prescribed was 252 (18.5%). Aceclofenac + paracetamol prescribed were 169 (12.4%), followed by paracetamol + tramadol prescribed were 78 (5.72%), and loraxicam + paracetamol prescribed were 5 (0.36%) Figure 3.
|
|
|
Figure 3. Distribution of combinational therapy of analgesics |
The Pattern of Analgesics Prescribed for Topical Application (Ointments)
In our study, out of 552 (40.5%), topical applications - diclofenac gel prescribed was about 111 (8.14%) under various brand names such as spafast gel, swift gel, bestnac gel, molliplus gel, dolorace gel.
The Pattern of Analgesics Prescribed for Parenteral Administration (Injections)
Our study shows that 552 (40.5%) of total analgesics were prescribed, and only 18 (1.32%) were parenteral preparations. Out of 18 (1.32%), diclofenac injection accounts for about 16 (1.17%), which were prescribed under the brand names spafast-D 15 (1.10%) & nugesic AQ 1 (0.07%). The tramadol prescribed was 2 (0.14%), an opioid analgesic.
The Pattern of Adjuvants Prescribed for the Study Population
An adjuvant is any substance, whether a drug, another substance, or a combination of the two, used to increase the effectiveness or potency of a particular medication. In our study, the adjuvants used are anticonvulsants, antidepressants, anesthetic agents, skeletal muscle relaxants given in combination with analgesics as a single drug, steroids, antibiotics, hormones, and bisphosphonates.
The Pattern of Anti-Coagulants Prescribed
In our study, out of total drugs (1362), anticonvulsants alone and a combination of anticonvulsants with other drugs such as antidepressants, Vit-B12, and anaesthetic agents account for about 186 (13.65%).
Monotherapy of anticonvulsants prescribed accounts for about 51 (3.74%). Where pregabalin - 75mg prescribed was 49 (3.59%) and pregabalin – 50mg prescribed was 1 (0.07%), Gabapentin prescribed was 1 (0.07%).
The Pattern of Combinational Therapy of Anticonvulsants with Methylcobalamin (An Active Form of Vit-B12) and Mecobalamin (One of the Coenzyme Forms of Vit-B12) Prescribed
Combinational therapy of anticonvulsants with methycobalamin prescribed was57 (4.18%). Pregabalin + methylcobalamin prescribed were 50 (3.67%), followed by gabapentin + metylcobalamin prescribed were 7 (0.51%). Combination of pregabalin + mecobalamin.
The Pattern of Combinational Therapy of Anticonvulsants with Antidepressants Prescribed
Combinational therapy of anticonvulsants with antidepressants prescribed were 36 (2.64%). Among them, gabapentin + nortriptyline prescribed were 32 (2.34%), followed by pregabalin + nortriptyline prescribed 3 (0.22%), clonazepam + escitalopram prescribed was 1 (0.07%).
The Pattern of Combinational Therapy of Anticonvulsants with Antidepressants and Methylcobalamin Prescribed
Combinational therapy of anticonvulsants with antidepressants and metylcobalamin prescribed was 36 (2.64%). Among them, gabapentin + methylcobalamin + nortriptyline prescribed were 31 (2.27%), followed by pregabalin + methylcobalamin + nortriptyline prescribed were 5 (0.36%).
The Pattern of Combinational Therapy of Anticonvulsants with an Anesthetic Agent
Combinational therapy of anticonvulsants with an anesthetic agent (lidogaba gel – Gabapentin + lidocaine) prescribed was 1 (0.07%).
The Pattern of Antibiotics Prescribed
In our study, out of the total drugs (1362), total antibiotics prescribed were about 45 (3.30%). Cefuroxime + clavulanic acid prescribed was13 (0.95%), cefuroxime prescribed was9 (0.66%), amoxicillin + potassium clavunate prescribed was6 (0.44%), linezolid prescribed was about 4 (0.29%), doxycycline prescribed were about 2 (0.14%), cephalexin + clavunate prescribed was only 1 (0.07%).
Among them, 35(2.6%) were prescribed in tablet form, (0.44%) were prescribed in injection form either i.v or i.m, 3(0.22%) were prescribed in powder form (gastolac sachets), 1 (0.07%) was prescribed in ointment form.
The Pattern of Nutritional Supplements Used as Adjuvants in the Management of Pain
The pattern of nutritional supplements which is enriched with collagen peptide, chondroitin sulfate, sodium hyaluronate, glucosamine, diacerin, and vitamins prescribed:
In our study, the prescribed drugs that improve the function of joints by reducing stiffness and pain in the joints in conditions such as osteoarthritis, trigger finger thumbs, etc., are prescribed at about 67 (4.9%).
The Pattern of Calcium, Vit – D3, and Multivitamins, Minerals Prescribed
In our study, out of 1362 prescribed drugs, 143 (10.49%) were calcium, vit – D3, multivitamins, and minerals. Among them, 137 (10.05%) were prescribed in tablet form, 1 (0.07%) was prescribed in powder form, 4 (0.29%) were prescribed in syrup form and 1 (0.07%) in injection form.
The Pattern of Corticosteroids Prescribed
Out of the total drugs prescribed, corticosteroids account for only about 40 (2.93%), where deflazacort prescribed was 26 (1.90%), and prednisolone prescribed was 14 (1.0%).
The Pattern of Hormonal Perpetration Prescribed
The hormonal preparation that is used as an adjuvant in the treatment of osteoporosis in our study was teriparatide (a man-made version of parathyroid hormone) with a brand name in. Bonista prescribed were 2 (0.14%).
The Pattern of Bisphosphonates Prescribed
Bisphosphonates that are used as an adjuvant in the treatment of osteoarthritis in our study were idrofos 150 mg (Ibandronate) prescribed were 2 (0.14%).
The Pattern of Antidepressants Prescribed
In our study, the antidepressants prescribed were 2 (0.14%). Among them, amican 10 (amitriptyline) prescribed was 1 (0.07%), which is a tricyclic antidepressant, and dulotin 20 (duloxetin) prescribed was (0.07%), which is an SNRI (serotonin-norepinephrine reuptake).
The Pattern of DMARDS Prescribed
DMARDs are used as adjuvants as they decrease the inflammation and pain in rheumatoid arthritis and several inflammatory conditions. The DMARDs prescribed in our study were 37 (2.71%). Among them, hydroxyl chloroquine prescribed was 25 (1.83%), methotrexate prescribed was 7 (0.51%), and sulfasalazine prescribed was 5 (0.36%).
The Pattern of Other Drugs Prescribed in Our Study
Drugs other than analgesics and adjuvants used in our study were antiulcer agents, antihistamines, antiemetics, and emollients.
The Pattern of Anti-Ulcerative Agents Prescribed
The total anti-ulcerative agents prescribed were 271 (19.89. Among them, drugs prescribed in tablet form were 267 (19.60%), drugs prescribed in injection form were 2 (0.14%), and drugs prescribed in syrup form were 2 (0.14%).
Rabeprazole + domperidone prescribed were 193 (14.17%) under various brand names, pantaprazole prescribed were 43 (3.15%), esomeprazole + domperidone prescribed were 5 (0.36%), and pantaprazole + domperidone prescribed were 26 (1.96%).
Drugs prescribed in injection form were 2 (0.14%), which was pantoprazole, and in syrup form was aristozyme (contains digestive enzymes) prescribed 2 (0.14%).
Other Drugs Prescribed
Other drugs prescribed were only 5 (0.36%). Among the antihistamines (cinnarizine) prescribed were 2 (0.14%), antiemetic (ondansetron) prescribed were 1 (0.07%) and anti-helminthic (diethylcarbamazine) prescribed were 2 (0.14%).
Drug Usage Problems and Side Effects Caused in Our Study
Analgesics
Because of the high intensity of pain, some patients (14 patients) used analgesics (paracetamol and tramadol combination – 9 patients, diclofenac – 5 patients) more than prescribed; the usual side effect of analgesics was conditions of excess stomach acid secretion and irritation of stomach which are controlled with anti-ulcerative agents.
Calcium Supplements
Calcium can cause side effects like belching, so some patients (24 patients) had less than prescribed.
DMARDS
Among DMARDS, methotrexate should be used only once a week, so some patients (2 out of 6 patients prescribed with methotrexate) have missed the dose. While using methotrexate, folic acid has been prescribed as a supplement because methotrexate is a folate antagonist.
Drug-Drug Interactions
In our study, corticosteroids are prescribed along with NSAIDS as a synergistic effect, where corticosteroids decrease pain by reducing inflammatory mediators and analgesics. This was seen in 32 prescriptions. However, this drug interaction is also harmful, which increases the risk of peptic ulcers, so they were prescribed anti-ulcerative agents.
The drug utilization analysis of analgesics and adjuvants used in pain management in various dosage forms, such as tablets, injections (IV, IM), powder form, and topical solutions to relieve pain, was further clarified by our study. Tablets are the most often prescribed medication for 377 patients. Certain tablets are used as combination therapy, while others are used as monotherapy. The adjuvants utilized in the current data include steroids, antibiotics, hormones, bisphosphates, anesthetic agents, anticonvulsants, antidepressants, and skeletal muscle relaxants administered in combination with analgesics as single medications. Most of the patients in this case study were administered diclofenac orally, topically, and intravenously. The most often prescribed combination medications are cefuroxime + clavulanic acid and aceclofenac + paracetamol.
The gender distribution reveals that, in comparison to men, women were more impacted. Across all age groups of analgesics and adjuvants considered, the amount of prescribed medication increased significantly with the severity of pain. However, of those with identified severe pain, 27.5% did not have access to prescription painkillers. Compared to elderly teenagers, residents over 85 years old were less likely to be prescribed analgesics or adjuvants.
There are some common pains in patients who visit the hospital that are classified as mild, moderate, and severe pain based on clinical manifestations for prescribing analgesics. The numerical rating scale (NRS) uses an 11-point scale ranging from 0- "no pain" to 10- "worst possible pain." This Pain intensity can be assessed both during and after treatment. The majority of patients complain of lower back pain; one-third of patients have tibia pain; arthritis such as rheumatoid arthritis, osteoarthritis, and septic arthritis; cellulitis; osteoporosis; synovitis; plantar fascitis; and other pains such as myalgias, fibromyalgia, and post-viral arthralgia, among others.
CONCLUSION
This study shows that monotherapy and combination therapy with non-opioid medications like diclofenac can effectively reduce pain. Patients who could not get pain relief from diclofenac alone were given opioid analogs (tramadol), tramadol combined with paracetamol. Analgesic use was discovered to depend on the patient's age and the type of surgery. Providing post-operative patients with good and efficient pain control will be feasible through the responsible and safe use of analgesics. Increasing knowledge of the RATIONAL usage OF DRUGS and routine prescription auditing will be helpful for the improvement of correct drug usage, which in turn can deliver high-quality healthcare at a low cost. This utilization study was conducted to lay the groundwork for a more in-depth investigation into the prescribing patterns of analgesic medications in academic medical centers. This study reveals a pattern of analgesic use that includes the utilization of large oral analgesic preparations, a high generic naming of medications, and the appropriate use of these pharmaceuticals regarding the dosage strength, the frequency of administration, and the treatment period.
ACKNOWLEDGMENTS: The authors would like to thank Dr. T. Gopalakrishnaiah, MS Ortho, senior consultant Orthopaedic Surgeon, GK Speciality Hospital, Pogathota, Nellore for providing permission to conduct this study.
CONFLICT OF INTEREST: None
FINANCIAL SUPPORT: None
ETHICS STATEMENT: The study was approved by the Institutional Ethics Committee of A C Subba Reddy Government Medical College & Hospital Dargamitta, Nellore 524004 Andhra Pradesh, India with a reference number Regd No: ECR/961/Inst/AP/2017/RR-20.
References
- Lumley MA, Cohen JL, Borszcz GS, Cano A, Radcliffe AM, Porter LS, et al. Pain and emotion: A biopsychosocial review of recent research. J Clin Psychol. 2011;67(9):942-68. doi:10.1002/JCLP.20816
- Jongchanapong A, Thongphichai W, Wasana PW, Sukrong S, Suttisri R, Amnuoypol S, et al. Antinociceptive efficacy of Clerodendrum petasites S. Moore, a Thai medicinal plant, and its CNS safety profiles. J Tradit Complement Med. 2023;13(1):81-92. doi:10.1016/J.JTCME.2022.11.001
- Craig KD. A child in pain: A psychologist’s perspective on changing priorities in scientific understanding and clinical care. Paediatr Neonatal Pain. 2020;2(2):40-9. doi:10.1002/PNE2.12034
- Barber TX. Toward a theory of pain: Relief of chronic pain by prefrontal leucotomy, opiates, placebos, and hypnosis. Psychol Bull. 1959;56(6):430-60. doi:10.1037/H0046676
- Mitchell SA, Majuta LA, Mantyh PW. New insights in understanding and treating bone fracture pain. Curr Osteoporos Rep. 2018;16:325-32. doi:10.1007/S11914-018-0446-8
- Woo AK. Depression and anxiety in pain. Rev Pain. 2010;4(1):8-12. doi:10.1177/204946371000400103
- Raja SN, Carr DB, Cohen M, Finnerup NB, Flor H, Gibson S, et al. The revised international association for the study of pain definition of pain: Concepts, challenges, and compromises. Pain. 2020;161(9):1976-82. doi:10.1097/J.PAIN.0000000000001939
- Apkarian AV, Baliki MN, Farmer MA. Predicting transition to chronic pain. Curr Opin Neurol. 2013;26(4):360-7. doi:10.1097/WCO.0B013E32836336AD
- Borsheski R, Johnson QL. Pain management in the geriatric population. Mo Med. 2014;111(6):508-11.
- Voepel-Lewis T, Zanotti J, Dammeyer JA, Merkel S. Reliability and validity of the face, legs, activity, cry, consolability behavioral tool in assessing acute pain in critically ill patients. Am J Crit Care. 2010;19(1):55-61. doi:10.4037/AJCC2010624
- Singh VK, Shetty YC, Salins N, Jain P. Prescription pattern of drugs used for neuropathic pain and adherence to NeuPSIG guidelines in cancer. Indian J Palliat Care. 2020;26(1):13-8. doi:10.4103/IJPC.IJPC_172_19
- Aggarwal R, Ranganathan P. Study designs: Part 2–descriptive studies. Perspect Clin Res. 2019;10(1):34-6. doi:10.4103/PICR.PICR_154_18
- Abdolrazaghnejad A, Banaie M, Tavakoli N, Safdari M, Rajabpour-Sanati A. Pain management in the emergency department: A review article on options and methods. Adv J Emerg Med. 2018;2(4):e45. doi:10.22114/AJEM.V0I0.93
- In J. Introduction of a pilot study. Korean J Anesthesiol. 2017;70(6):601-5. doi:10.4097/KJAE.2017.70.6.601
- Gordon DB, Dahl JL, Miaskowski C, McCarberg B, Todd KH, Paice JA, et al. American pain society recommendations for improving the quality of acute and cancer pain management: American pain society quality of care task force. Arch Intern Med. 2005;165(14):1574-80. doi:10.1001/ARCHINTE.165.14.1574
- Fernandes CM. Emergency department overcrowding: What is our response to the “new normal”? Acad Emerg Med. 2003;10(10):1096-7. doi:10.1111/J.1553-2712.2003.TB00580.X
- Patino CM, Ferreira JC. Inclusion and exclusion criteria in research studies: Definitions and why they matter. J Bras Pneumol. 2018;44:84. doi:10.1590/S1806-37562018000000088
- Montes de Oca M, Menezes A, Wehrmeister FC, Lopez Varela MV, Casas A, Ugalde L, et al. Adherence to inhaled therapies of COPD patients from seven Latin American countries: The LASSYC study. PloS one. 2017;12(11):e0186777. doi:10.1371/JOURNAL.PONE.0186777
- Al Jundi A, Sakka S. Protocol writing in clinical research. J Clin Diagn Res. 2016;10(11):ZE10-3. doi:10.7860/JCDR/2016/21426.8865
- Toy A, Eaton KA, Santini A. An introduction to research for primary dental care clinicians: Part 2: Stage 4. Planning the Study. Prim Dent Care. 2011;18(1):36-40. doi:10.1308/135576111794065810
- Farahmand S, Shafazand S, Alinia E, Bagheri-Hariri S, Baratloo A. Pain management using acupuncture method in migraine headache patients; A single blinded randomized clinical trial. Anesthesiol Pain Med. 2018;8(6):e81688. doi:10.5812/AAPM.81688