Archive \ Volume.15 2024 Issue 2
Impact of Telemedicine on the Clinical Outcomes among Elderly Patients: A Systematic Review
Abstract
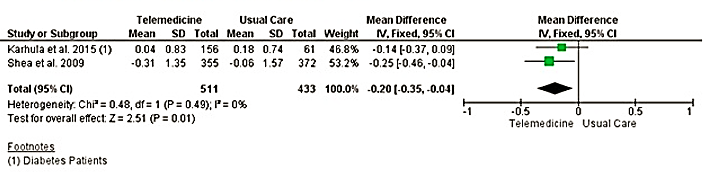
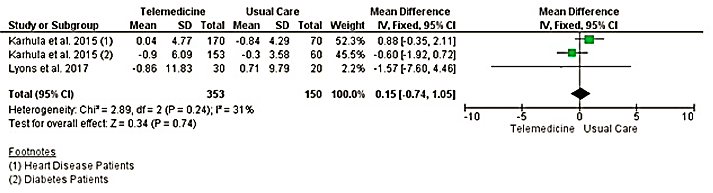
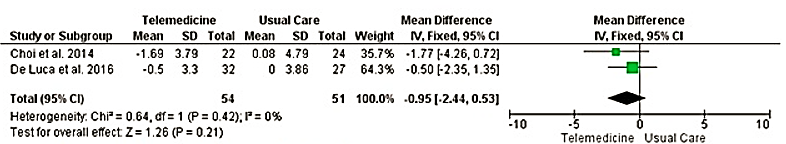
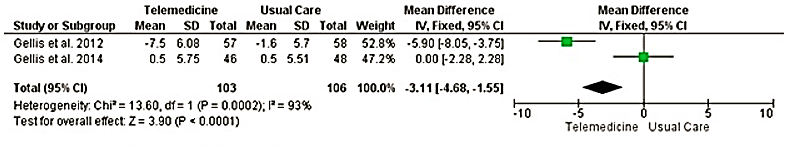
Telemedicine has been increasingly used in the provision of health care services to older adults. The objective of this study was to investigate the impact of telemedicine use on clinical and self-reported outcomes of older patients through systematic review and meta-analysis. Online search was made from PubMed, psycINFO, Scopus, Ovid (Embase, Emcare), and EBSCOhost for randomized controlled trials and quasi-experimental studies evaluating the effect of telemedicine on clinical and self-reported outcomes of older patients (age>60 years). A total of seven studies were included in this review. Among the clinical outcomes, telemedicine had a statistically significant effect on systolic blood pressure (-3.83; 95% CI [-6.04, -1.61]; I2=77%;p=0.001) and glycosylated hemoglobin (-0.20; 95% CI [-0.35, -0.04]; I2=0; p=0.01). Whereas, no significant effect was observed for diastolic blood pressure (-0.92;95%CI [-2.14,0.30]; I2 0%; p=0.44), low-density lipoprotein (-0.01; 95%CI [-0.09,0.07]; I2=0%;p=0.930), and body weight (0.15;95%CI [-0.74,1.05]; I2 =0%;p=0.420. Depressive symptoms rating was assessed using two different measurement tools, Geriatric Depression Scale (GDS) and Patient Health Questionnaire 9 (PHQ-9). Significant effect was reported with PHQ-9 (-3.11;95%CI [-4.68,-1.55];I2=93%;p=0.0002). Results from this systematic review suggest that key clinical outcomes and health behavior of older patients can be improved using telemedicine.
How to cite:
Download Citation
INTRODUCTION
Telehealth or telemedicine represents a method of providing health care services by using the currently available information communication technology (ICT) which allows patients to access health care services from a distance. Such technology allows patients to receive health care without needing to visit a doctor’s clinic, hospital, or any other health care facility unless the treatment of the patient’s condition necessitates the physical presence of a health care professional [1, 2]. The World Health Organisation (WHO) defines telemedicine as the provision of health care services through long-distance interaction between all health care professionals and the patient to discuss health matters pertaining to the patient’s diagnosis, treatment, and disease management or for research and evaluation by utilizing ICT to improve the health outcomes of individual patients and the community as a whole [3].
In 2017, the United Nations (UN) estimated the population of older people aged 60 or above, to be at 962 million which comprised 13% of the total world population [3]. The proportion of the older population is expected to increase from 1.4 billion in 2030 to 2.1 billion in 2050. The rise in the number of individuals in this age group raises many concerns particularly in the field of health care due to the prevalence of comorbidities and chronic conditions in older adults. The prevalence of multi-morbidity and polypharmacy rises with increasing age, particularly amongst those 60 years and older [4]. Thus, the treatment and healthcare of patients from the older age group have become increasingly challenging and demand a large proportion of resources from the healthcare system. Furthermore, the cost and expenditure for the treatment of chronic conditions which are more prevalent amongst older people will be expected to further increase along with the growth of this population [5].
Therefore, telemedicine is a promising avenue that could help reduce the cost of healthcare and the burden on the healthcare system from this population while improving their health benefits. The use of telemedicine has been shown to have promising benefits to patients using already available healthcare systems [6-16]. Thus, the introduction of telemedicine into the healthcare of older adults has the potential to serve as a new platform to educate older patients on health and disease management while being meticulously monitored by healthcare professionals. This would be able to improve self-care amongst older patients which would reduce the reliance of patients on healthcare professionals for minor health issues. The increased possibility of early detection of chronic diseases would promote earlier treatment and improve clinical outcomes for older patients.
Previous research [17-19] provides evidence that the implementation of telemedicine in health care stands to significantly reduce costs and unnecessary expenditures. The utilization of telemedicine is seen to improve patient compliance and lower unneeded use of resources, which in turn helps to cut down expenses on health care. However, the impact of telemedicine on clinical and self-reported outcomes of older patients has not been fully reviewed systematically.
Objective
The objective of this systematic literature review is to evaluate the impact of telemedicine and other forms of remote monitoring technology on the clinical and self-reported outcomes of older patients. In doing so, the effectiveness and feasibility of the use of telemedicine and remote monitoring technology can be assessed to determine the value of this technology in the field of healthcare.
MATERIALS AND METHODS
Search Strategy
A systematic search was conducted across six databases namely, PubMed, EMBASE (Ovid), EMCARE (Ovid), PsycINFO, and EBSCOhost by two independent reviewers using key phrases related to the research question as search terms. The terms ‘Geriatrics’, ‘Well-being’, and ‘Technology’ were used together with the Boolean phrase ‘AND’, along with alternative phrases that are synonymous with the key terms mentioned. Further description of the search strategy and the list of alternative phrases used. The same phrases were used as search terms for every database. The terms were searched in all fields without having any restrictions in the year of publication, field of study, or any other search criteria.
Inclusion and Exclusion Criteria
The studies were included in the review if there were: 1) addressing the use of technology and the health outcome of older patients (60 years and older), 2) Measuring the effects of telemedicine or remote monitoring technology on any of the clinical or patient’s self-reported outcomes; and 3) randomized controlled trials and quasi-experimental studies. Non-English language papers were excluded. We used the taxonomy of classification of telemedicine as described in a previous study [20].
Study Selection
Articles were screened with the study titles followed by abstract and full-text screening.
Data Extraction Process
Data were extracted independently on the study characteristics, the study population, interventions, and outcomes using Google spreadsheets. Quantitative results from randomized controlled trials in the form of continuous and binary data were collected and sorted in separate sheets.
Quality Assessment
The quality of the studies that were selected to be included in the study was assessed and examined by one independent reviewer using the Cochrane Risk of Bias Tool [21]. Each criterion for each study was rated ‘low risk’ if there was a low chance of any bias or a low possibility that the existence of any bias would significantly affect the outcome of the study, ‘high risk’ if there was a high chance of any bias or a high possibility that the existence of any bias would significantly affect the outcome of the study, and ‘unclear risk’ if the existence of any bias in the study could not be determined due to particular reasons. The quality assessment was cross-checked by another independent reviewer by reviewing the assessment of three studies. There were no major issues or disputes brought up during the cross-check and the initial assessment of the quality of the included studies was retained.
Outcomes of Interest
The clinical outcomes included changes in blood pressure (measured in mmHg), low-density lipoprotein (LDL) blood levels (measured in mmol/L), body weight (measured in kg), and HbA1c levels (measured in %). The self-reported outcomes consisted of depression and health-related quality of life (HRQoL). Depression was assessed using the Geriatric Depression Scale (GDS) and Patient Health Questionnaire 9 (PHQ-9), whereas HRQoL was assessed by using the 36-Item Short Form Survey (SF-36). Only three components of the SF-36 were included in this systematic review, namely measures of bodily pain, general health, and social functioning.
Analysis
Results obtained involving clinical outcomes which included changes in blood pressure (systolic and diastolic blood pressure), LDL blood levels, HbA1c blood levels, and body weight along with self-reported patient outcomes which included depression and quality of life ratings were assessed through meta-analysis. The Review Manager 5.3 program was used to conduct the meta-analyses for each of the individual outcomes of interest by using a random effects model.
RESULTS AND DISCUSSION
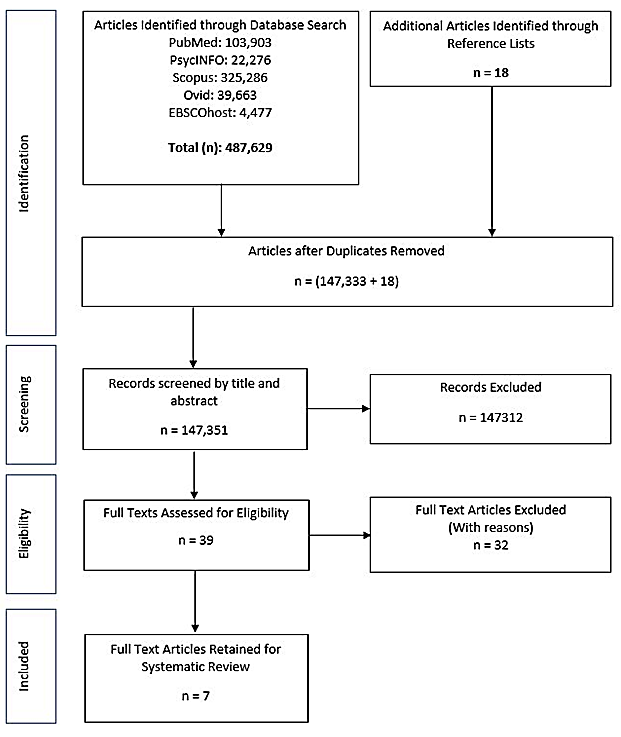
A total of 147,333 unique titles were screened, followed by abstract screening and full-text screening (n=39). A total of seven studies were included (Figure 1).
|
|
|
Figure 1. PRISMA Flow Diagram |
Description of Included Studies
All the included studies (n=7) were published between year 2009 to 2017 [22-28]. There was one quasi-experimental study among the included articles Choi et al. (2014) [22], the other six studies were randomized controlled trials [23-28]. Four of the included studies were conducted in the United States [24, 25, 27, 28] while the other three studies were each conducted in Korea [22, 23, 26].
Clinical outcomes that included changes in blood pressure (systolic and diastolic blood pressure), LDL blood levels, HbA1c levels, and body weight were evaluated in five studies [22, 23, 26-28] whereas, self-reported patient outcomes including depression and quality of life were evaluated in five studies [22-26].
The comorbid conditions of the study population were specified in three of the included studies whereby one study evaluated chronically ill and depressed older patients primarily [25], the second study investigated heart disease patients and COPD patients [24], and the third study examined heart disease patients and diabetic patients [26]. However, patients in all three of the studies were reported to have multiple comorbidities besides the primary chronic illnesses being studied [24-26]. A detailed description of all the included studies in this review has been provided in Table 1.
|
Table 1. Main Study Characteristics of Included Studies |
|||||||
|
Study |
Region & Country |
No. of Participants (n) Lost to Follow-up (n) Age in Year (Mean [SD]) Gender (% Female) |
Follow-up Duration |
Comorbi-dities |
Intervention |
Control |
Outcome Measures |
|
Choi et al. (2014) [22] |
Seoul, Korea |
No. of Participants (IG/CG): 25/24 Lost to Follow-up (IG/CG): 0/1 Age (IG/CG): 71.46 [6.17]/71.42 [5.14] Sex (IG/CG): 68%/62.5% |
8 weeks |
NR |
The experimental group received remote consultation twice a week. The consultation was mainly related to blood pressure monitoring, which included a blood pressure check, drug intake and clarification of events that may have affected their blood pressure |
The control group received regular treatment. There was no further mediation after the installation of the equipment and the initial training |
SBP, DBP, depression status, healthy lifestyle |
|
De Luca et al. (2016) [23] |
Messina, Italy |
No. of Participants (IG/CG): 32/27 Lost to Follow-up (IG/CG): 0/0 Age (IG/CG): 77 (71 – 80)/ 85 (79 – 89) Sex (IG/CG): 65.6%/70.4% |
2 years |
NR |
The patients in the experimental group were monitored for vital signs three times per week, and received a weekly consultation either by a neurologist or a psychologist
|
Patients received standard in-home nursing care |
SBP, DBP, depression, HRQoL |
|
Gellis et al. (2012) [24] |
New York, United States |
No. of Participants (IG/CG): 58/57 Lost to Follow-up (IG/CG): 3/7 Age (IG/CG): 80.1 [7.8]/78.3 [6.9] Sex (IG/CG): 63.16%/68.97% |
3 months & 12 months |
HF, COPD, DM, Hypertension, Osteoarthritis |
The telehealth monitoring system was provided to home care patients to enhance the patients' self-management of their medical condition. Patients obtained education on the disease process and counselling
|
Participants received standard home care services provided by registered nurses in the role of case managers plus health education |
ED visits, duration of hospitalization, depression status, satisfaction |
|
Gellis et al. (2014) [25] |
Pennsylvania, United States |
No. of Participants (IG/CG): 58/57 Lost to Follow-up (IG/CG): 3/7 Age (IG/CG): 80.1 [7.8]/78.3 [6.9] Sex (IG/CG): 63.16%/68.97% |
6 months & 12 months |
HF, COPD, DM, Hypertension, Osteoarthritis |
Participants were assigned an I-TEAM nurse within 5 days of referral. I-TEAM nurses were restricted to providing services to I-TEAM participants. Intervention included: telemonitoring, chronic illness and depression case management, and PST for depression
|
Usual care was provided to patients augmented with psychoeducation. Usual care nurses conducted 1-hour-long face-to-face home visits at least weekly over a 3-month period |
Satisfaction, Depression status, HRQoL, ED visits |
|
Karhula et al. (2015) [26] |
Eksote, Finland |
No. of Participants (IG/CG) (HD): 190/79 No. of Participants (IG/CG) (D): 180/70 Lost to Follow-up (IG/CG): 33/15 Age (IG/CG) (HD): 69.6 [9.1]/68.1 [9.4] Age (IG/CG) (D): 66.6 [8.2]/65.5 [9.6] Sex (IG/CG) (HD): 34.74%/31.65% Sex (IG/CG) (D): 45.0%/42.86%
|
1 year |
Heart Disease, Cerebrovascular Disease, COPD, Connective Tissue Disease, DM, Cancer |
The intervention consisted of health coaching over mobile phones and self-monitoring of health parameters with the help of a RPM system |
Patients received the care they would have received in the absence of the study. As part of the standard care, patients received a disease management booklet at the time of diagnosis. Patients can contact health care services any time they feel they need to |
HRQoL, HbA1c, SBP, DBP, body weight, waist circumference, adherence, LDL, HDL, total cholesterol, triglycerides |
|
Lyons et al. (2017) [27] |
Texas, United States |
No. of Participants (IG/CG): 30/20 Lost to Follow-up (IG/CG): 1/1 Age (IG/CG): 61.25 [5.00]/61.70 [6.26] Sex (IG/CG): 85.0%/85.0% |
12 weeks |
NR |
The participants randomized to the intervention group were lent a mini tablet mobile device and a wearable electronic activity monitor for home use during the study. Weekly telephone counselling with goal setting was provided.
|
The wait list control group did not receive any intervention until after their final assessment, when they were provided the intervention in full |
Stepping time per day, steps per day, sitting time per day, body fat, body weight, fitness |
|
Shea et al. (2009) [28] |
New York, United States |
No. of Participants (IG/CG): 844/821 Lost to Follow-up (IG/CG): 514/358 Age (IG/CG): 70.8 [6.5]/70.9 [6.8] Sex (IG/CG): 63.51%/62.12% |
5 years |
NR |
Patients received a HTU with four main functions: synchronous videoconferencing, self-monitoring of fingerstick glucose and blood pressure, messaging and Web access. The nurse case managers are trained in diabetes management and in the use of computer-based case management tools that facilitate interactions through videoconferencing with patients |
Patients in the usual care group received clinical care from their primary care providers, without other guidance or direction from study personnel |
SBP, DBP, HbA1c, LDL, mortality |
Description of Interventions
The interventions of the included studies were provided by a range of primary healthcare professionals, such as nurses, general practitioners, psychologists, and neurologists. All seven of the included studies had teleconsultation, videoconferencing, or teleconferencing as part of the intervention for the telemedicine group of patients. A remote monitoring system to observe the symptoms of certain diseases or regular physiological measurements as part of the intervention was included in all included studies. Education about the patients’ chronic illness or general health was only provided as part of the intervention two studies [24, 25]. One study [27] included goal setting and action planning by a health coach or primary healthcare provider as part of the intervention for the telemedicine group of patients. The details of interventions given to the telemedicine group and usual care group are provided in Table 1.
Quality of Included Studies
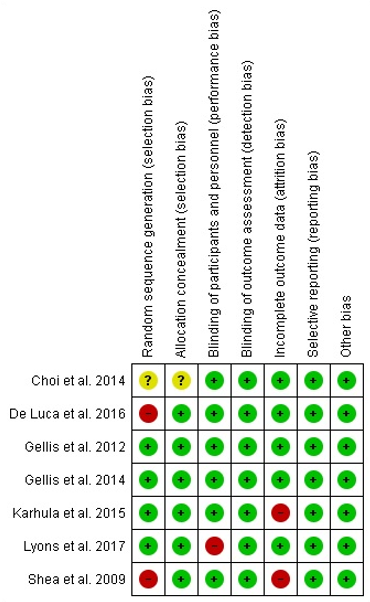
Overall, the results and outcomes from the included studies possess high reliability as more than 50% of the studies reported a low risk of bias in each criterion assessed. Three of the included studies were likely to have a high risk of bias in terms of random sequence generation [23, 28], while one study had unclear random sequence generation [22]. The random sequence generation represented the major source of any possible bias among all the components that were assessed, with only four studies (57.1%) reporting a low risk of bias [24-27], two studies reporting a high risk of bias [23, 28] and one study having an unclear risk of bias [22]. All seven studies included in this systematic review reported a low risk of bias for blinding of outcome assessment, selective reporting, and any other source of bias [22-28]. The general summary of the quality assessment and risk of bias of each study are presented in Figure 2, respectively.
|
|
|
Figure 2. Risk of Bias from the Selected Studies |
Clinical Outcomes
Blood Pressure
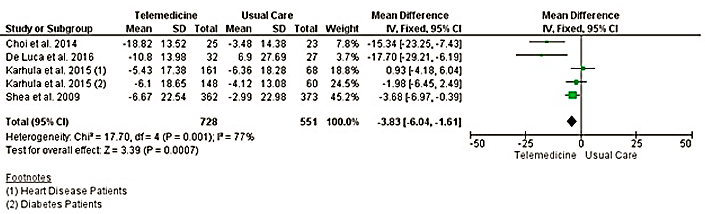
Blood pressure was measured as systolic blood pressure and diastolic blood pressure in four studies [22, 23, 26, 28]. The mean change of systolic blood pressure from baseline to follow-up for the control groups and intervention groups in each study ranged from -4.12 mmHg to +6.9 mmHg and -18.82 mmHg to -5.43 mmHg respectively (Figure 3). The results of the meta-analysis showed a statistically significant reduction of systolic blood pressure -3.83 (95% CI -6.04, -1.61) as compared to usual care (Table 2). Whereas no significant reduction was observed for diastolic blood pressure (-0.92; 95%CI -2.14, 0.30) (Figure 3).
|
Table 2. Pooled clinical and self-reported patient outcomes |
|
|
Outcome |
Pooled results MD(95% CI) |
|
Clinical Outcomes |
|
|
Blood Pressure (mmHg) |
|
|
Systolic Blood Pressure |
-3.83 (-6.04, -1.61) |
|
Diastolic Blood Pressure |
-0.92 (-2.14, 0.30) |
|
Blood LDL Levels (mmol/L) |
-0.01 (-0.09, 0.07) |
|
HbA1c (%) |
-0.20 (-0.35, -0.04) |
|
Body Weight (kg) |
+0.15 (-0.74, 1.05) |
|
Self-Reported Patient Outcomes |
|
|
Depression |
|
|
GDS |
-0.95 (-2.44, 0.53) |
|
PHQ-9 |
-3.11 (-4.68, -1.55) |
|
HRQoL |
|
|
Bodily Pain |
-0.22 (-3.69, 3.25) |
|
General Health |
+2.33 (-0.36, 5.02) |
|
Social Functioning |
-0.25 (-4.01, 3.51) |
MD = mean difference; CI = confidence interval; GDS = Geriatric Depression Scale; PHQ = Patient Health Questionnaire 9; HRQoL = Health Related Quality of Life.
|
|
|
a) Systolic blood pressure |
|
|
|
b) Diastolic blood pressure |
|
|
|
c) Blood cholesterol (low density Epoprotcine) |
|
|
|
d) Glycated haemoglobin |
|
|
|
e) Body weight |
|
Figure 3. Forest Plots on systolic blood pressure, diastolic blood pressure, blood cholesterol, glycated haemoglobin and body weight. |
Blood LDL Levels
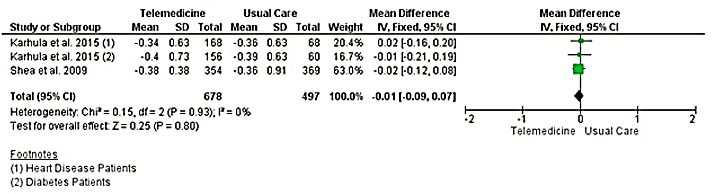
Two studies evaluated blood LDL levels as a clinical outcome [26, 28]. The control groups and intervention groups from both studies had a mean change in blood LDL levels ranging from -0.36 mmol/L to -0.39 mmol/L and -0.34 mmol/L to -0.4 mmol/L respectively (Table 2). A statistically insignificant reduction in LDL was observed when compared to usual care (-0.01; 95% CI -0.09, 0.07) (Figure 3).
HbA1c
Two studies included HbA1c blood levels as an outcome of interest [26, 28]. There was a greater improvement in the mean changes of HbA1c in the intervention groups of both studies in comparison to the control groups. The mean changes from baseline to follow-up for the control groups in both studies were -0.06% and +0.18% while -0.31% and +0.04% were the mean changes for the intervention groups. Overall statistically significant reduction in HbA1c level was observed for telemedicine intervention (-0.2; 95% CI -0.35, -0.04) (Figure 3).
Body Weight
The body weight of patients was measured as a clinical outcome in two studies [26, 27]. Telemedicine interventions had an insignificant effect on the patient’s body weight (0.15; 95% CI: -0.74, 1.05) (Figure 3).
Self-reported Patient Outcomes
Depression
A total of four studies evaluated the depressive symptoms and depression status of older patients in relation to telemedicine usage in the delivery of healthcare [22-25]. Several tools were used to measure the depression ratings of patients across all four studies such as the Centre for Epidemiologic Studies Depression (CES-D), Geriatric Depression Scale (GDS), Hamilton Depression Scale (HAM-D), and the Patient Health Questionnaire-9 (PHQ-9), whereby some studies used more than one tool [22-25]. Since two different measurement tools were used by two studies each, a meta-analysis was conducted for both measurement tools in assessing the depressive symptoms of patients. The meta-analysis produced statistically significant results for the PHQ-9 measurement tool [24, 25] but not for the GDS measurement tool [22, 23] (Figure 4).
|
|
|
a) Depression (Geriatric Depression Scale) |
|
|
|
b) Depression (Patient Health Questionnaire-9) |
|
|
|
c) Quality of Life [SF-36(Bodily pain)] |
|
|
|
d) Quality of Life [SF-36(General Health)] |
|
|
|
e) Quality of Life [SF-36(Social Functioning)] |
|
Figure 4. Forest Plots on depression and quality of life. |
Telemedicine interventions had a statistically insignificant effect on the reduction of depression (-0.95 (95% CI: -2.44, 0.53), for the studies which used [22, 23]. However, a significant effect on depressive symptoms (-3.11; CI 95% CI -4.68, -1.55) was observed for PHQ-9 [24, 25] (Figure 4).
Health-Related Quality of Life (HRQoL)
Two out of the seven included studies measured and discussed HRQoL as an outcome [24, 26]. The HRQoL assessment in these two studies was done by using a 36-item Short Form Health Survey (SF-36). Bodily pain, general health, and social functioning were the three components of the SF-36 that were measured by both studies, whereby one of the studies recorded the values for two different groups of patients, heart disease patients and diabetic patients separately.
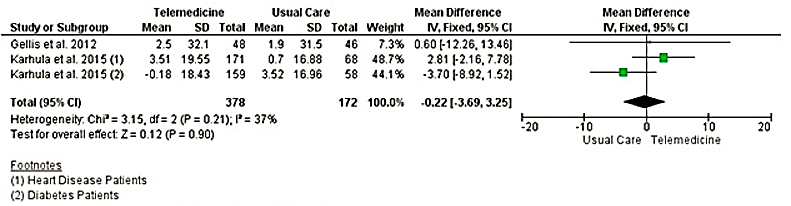
The scores for the bodily pain component in both studies had greater improvements in the intervention group than in the control group [24, 26]. However, the intervention group for the diabetic patients in one study did not have an improvement over the control group [26]. The mean change attained by the control groups and intervention groups in both studies ranged from +0.7 to +3.52 and -0.18 to +3.51 respectively. Results of the meta-analysis showed a statistically insignificant effect of telemedicine interventions on bodily pain (-0.22; 95% CI -3.69, 3.25), as compared to usual care (Figure 4).
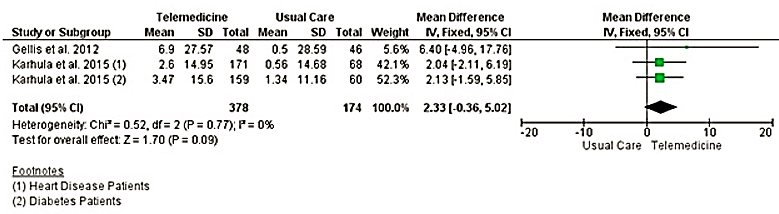
The intervention groups for both studies showed an improvement in the general health component scores than the control groups [24, 26]. The mean change for the control groups and intervention groups ranged from +0.5 to +1.34 and +2.6 to +6.9 respectively. However, according to meta-analysis, the improvement was statistically insignificant (2.33; CI 95% CI: -0.36, 5.02) (Figure 4).
For the social functioning domain of SF-36, the mean change in scores obtained by the control groups and intervention groups were in the range of -0.18 to +3.96 and +0.88 to +9.9 respectively. The telemedicine interventions had a statistically insignificant effect (-0.25; 95% CI -4.01, 3.51) on social functioning as compared to usual care (Figure 4).
The results from the included studies evaluated the effects of telemedicine on older patients for several clinical and patients’ self-reported outcomes, covering a wide range of comorbid conditions. The data analyzed from the included studies in this review has shown that telemedicine has the potential to improve certain areas of disease management.
In terms of disease management, the results showed a slight improvement in systolic blood pressure readings and HbA1c levels in older patients who are part of telemedicine programs as compared to older patients under usual care. Studies have shown that a decrease in systolic blood pressure may benefit patients with hypertension, risk of heart failure, diabetes mellitus, and other comorbidities [29-31]. This would be particularly beneficial for older patients who usually suffer from multiple comorbidities. Grossman (2011) [31] reported that a decrease in systolic blood pressure by 10 mmHg or 5 mmHg may reduce the risk of coronary artery disease events by 22% and lower the risk of stroke by 41%. Numerous studies have shown that reduction in blood HbA1c levels has been associated with improved clinical outcomes for diabetes patients [32-34]. One such study has reported that a reduction of HbA1c levels by 0.20% may potentially lower the risk of death by 10% [34]. This indicates that there have been improvements in the management of chronic conditions related to these two clinical outcomes such as hypertension, heart disease, and diabetes mellitus with the help of telemedicine.
Minor differences in changes in body weight in patients receiving telemedicine care in contrast to patients receiving usual care have been recorded. However, the results obtained from the meta-analysis of the two studies that measured body weight as a parameter were not statistically significant. There could be a possible explanation for this outcome as one of the two studies that reported changes in body weight as a clinical outcome which was conducted by Karhula et al. (2015) [26] had a greater emphasis on disease management during the intervention, with minor attention towards health behavior, particularly exercise. The study conducted by Lyons et al. (2017) [27] which had health behavior and exercise as the primary priority of the intervention produced an encouraging improvement in body weight of telemedicine patients as compared to usual care patients. Further studies may be conducted to determine the effectiveness of telemedicine on the exercise capacity of older patients as well. Healthy maintenance of regular exercise habits in older patients may reduce falling risks by improving their cognitive abilities and physical strength [35-37] and lowering the risk of death [38].
Effects on the mental health of older patients have only been assessed from one parameter which is depression or depressive symptom ratings using the GDS and PHQ-9 as measurement tools in four separate studies. Studies using the PHQ-9 as a measurement tool reported that the usage of telemedicine managed to improve the depressive symptoms in older patients by a significant amount whereas meta-analysis of the results obtained from the GDS measurement tool proved to be statistically insignificant Further studies should be conducted to assess the possible benefits of telemedicine on the mental health of older patients.
The HRQoL of older patients using telemedicine was assessed using three different components (bodily pain, general health, and social functioning) of the SF-36 measurement tool in two studies. However, the results obtained from the meta-analyses of these components from both of the involved studies were not statistically significant. Therefore, HRQoL and QoL represent important domains to be studied in regard to the implementation of telemedicine for older patients.
The use of telemedicine was able to efficiently educate older patients on the management of their comorbidities and served as a platform that allowed older patients to obtain advice or receive counseling regarding their comorbidities more regularly and frequently from healthcare professionals [22, 23, 28].
There appears to be limited literature on the use of telemedicine focused on the older patient population. In general, most of the studies analyzed in this review paper were conducted in the United States and European countries, with only one study conducted in Asia. There is a lack of evidence from low-resource settings. The use of telemedicine may provide a much greater impact in low-income countries whereby older patients have greater difficulty acquiring their required health care services. The study population in most of the included studies also consisted of mainly individuals who have ready access to medical facilities, nurse caregivers, or caretakers. Hence, more evidence is required regarding the impact of telemedicine on rural communities and other communities that have difficulty accessing healthcare facilities in order to better assess the value of telemedicine in providing healthcare services at a distance.
Quality assessment of the included studies has also revealed that some of the studies included in this systematic review have a high risk of bias or unclear risk of bias in certain areas (i.e. random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, and selective reporting). There is also a highly considerable degree of heterogeneity generated from a meta-analysis of some of the parameters such as systolic blood pressure (I2 = 77%), depression using the PHQ-9 measurement tool (I2 = 93%), and a moderate degree of heterogeneity for body weight (I2 = 31%), HRQoL – bodily pain (I2 = 37%). Therefore, the results analyzed in the meta-analysis are to be interpreted with more attention.
CONCLUSION
The results from this systematic review produce evidence that supports the use of telemedicine in facilitating geriatric care in older patients to improve overall disease management and health behavior. Findings from the meta-analysis conducted in this review paper show that the implementation of telemedicine in geriatric care has the potential to enhance the disease management and health behavior of older patients in terms of monitoring and managing blood pressure levels and HbA1c levels. Furthermore, improvements in mental health and HRQoL in older patients through the use of telemedicine are uncertain from the results attained in this systematic review and represent promising areas of study for the future. Overall, the use of telemedicine in the delivery of health care services has the potential for a positive impact on the disease management and health behavior of older patients.
ACKNOWLEDGMENTS: None
CONFLICT OF INTEREST: None
FINANCIAL SUPPORT: None
ETHICS STATEMENT: None
References
- Cannon NJ, Jurski K, Ulferts GW. Telemedicine. Am J Health Sci. 2014;5(2):95-102.
- Edwards JP. Dictionary of Nursing 6th Ed. Refer. 2014;30(1):22. Available from: http://www.oxfordreference.com.ezproxy.lib.monash.edu.au/view/10.1093/acref/9780199666379.001.0001/acref-9780199666379-e-8865
- Telemedicine WH. Opportunities and developments in member states. Geneva, Switzerland. 2010. Available from: http://apps.who.int/iris/bitstream/handle/10665/44497/9789241564144_eng.pdf;jsessionid=0E1E569EE94289E95B4A7530282FA369?sequence=1
- Hermans H, Evenhuis HM. Multimorbidity in older adults with intellectual disabilities. Res Dev Disabil. 2014;35(4):776-83.
- Ellison D, White D, Farrar FC. Aging population. Nurs Clin North Am. 2015;50(1):185-213.
- Au DH, Macaulay DS, Jarvis JL, Desai US, Birnbaum HG. Impact of a telehealth and care management program for patients with chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2015;12(3):323-31.
- Bashshur RL, Shannon GW, Smith BR, Alverson DC, Antoniotti N, Barsan WG, et al. The empirical foundations of telemedicine interventions for chronic disease management. Telemed J E Health. 2014;20(9):769-800.
- Chaudhry SI, Phillips CO, Stewart SS, Riegel B, Mattera JA, Jerant AF, et al. Telemonitoring for patients with chronic heart failure: A systematic review. J Card Fail. 2007;13(1):56-62.
- Clark RA, Inglis SC, McAlister FA, Cleland JG, Stewart S. Telemonitoring or structured telephone support programmes for patients with chronic heart failure: Systematic review and meta-analysis. BMJ. 2007;334(7600):942.
- Inglis SC, Clark RA, Dierckx R, Prieto-Merino D, Cleland JG. Structured telephone support or non-invasive telemonitoring for patients with heart failure. Cochrane Database Syst Rev. 2015;2015(10):CD007228.
- Kitsiou S, Paré G, Jaana M. Effects of home telemonitoring interventions on patients with chronic heart failure: An overview of systematic reviews. J Med Internet Res. 2015;17(3):e63.
- Dang S, Dimmick S, Kelkar G. Evaluating the evidence base for the use of home telehealth remote monitoring in elderly with heart failure. Telemed J E Health. 2009;15(8):783-96.
- Paré G, Jaana M, Sicotte C. Systematic review of home telemonitoring for chronic diseases: The evidence base. J Am Med Inform Assoc. 2007;14(3):269-77. doi:10.1197/jamia.M2270
- Chen K, Chan AH. Predictors of gerontechnology acceptance by older Hong Kong Chinese. Technovation. 2014;34(2):126-35.
- Kohlbacher F, Herstatt C, Levsen N. Golden opportunities for silver innovation: How demographic changes give rise to entrepreneurial opportunities to meet the needs of older people. Technovation. 2015;39:73-82.
- Yang HL, Hsiao SL. Mechanisms of developing innovative IT-enabled services: A case study of Taiwanese healthcare service. Technovation. 2009;29(5):327-37.
- Finkelstein SM, Speedie SM, Potthoff S. Home telehealth improves clinical outcomes at lower cost for home healthcare. Telemed J E Health. 2006;12(2):128-36.
- Minetaki K, Akematsu Y, Tsuji M. Effect of e-health on medical expenditures of outpatients with lifestyle-related diseases. Telemed J E Health. 2011;17(8):591-5.
- Noel HC, Vogel DC, Erdos JJ, Cornwall D, Levin F. Home telehealth reduces healthcare costs. Telemed J E Health. 2004;10(2):170-83.
- Lee SWH, Chan CKY, Chua SS, Chaiyakunapruk N. Comparative effectiveness of telemedicine strategies on type 2 diabetes management: A systematic review and network meta-analysis. Sci Rep. 2017;7(1):12680.
- Higgins JP. Cochrane handbook for systematic reviews of interventions. Version 5.1. 0 [updated March 2011]. The Cochrane Collaboration. www.cochrane-handbook.org. 2011.
- Choi H, Kim J. Effectiveness of telemedicine: Videoconferencing for low-income elderly with hypertension. Telemed J E Health. 2014;20(12):1156-64. doi:10.1089/tmj.2014.0031
- De Luca R, Bramanti A, De Cola MC, Trifiletti A, Tomasello P, Torrisi M, et al. Tele-health-care in the elderly living in nursing home: The first Sicilian multimodal approach. Aging Clin Exp Res. 2016;28(4):753-9.
- Gellis ZD, Kenaley B, McGinty J, Bardelli E, Davitt J, Ten Have T. Outcomes of a telehealth intervention for homebound older adults with heart or chronic respiratory failure: A randomized controlled trial. Gerontologist. 2012;52(4):541-52.
- Gellis ZD, Kenaley BL, Ten Have T. Integrated telehealth care for chronic illness and depression in geriatric home care patients: The integrated telehealth education and activation of mood (I-TEAM) study. J Am Geriatr Soc. 2014;62(5):889-95.
- Karhula T, Vuorinen AL, Rääpysjärvi K, Pakanen M, Itkonen P, Tepponen M, et al. Telemonitoring and mobile phone-based health coaching among finnish diabetic and heart disease patients: Randomized controlled trial. J Med Internet Res. 2015;17(6):e153.
- Lyons EJ, Swartz MC, Lewis ZH, Martinez E, Jennings K. Feasibility and acceptability of a wearable technology physical activity intervention with telephone counseling for mid-aged and older adults: A randomized controlled pilot trial. JMIR Mhealth Uhealth. 2017;5(3):e28.
- Shea S, Weinstock RS, Teresi JA, Palmas W, Starren J, Cimino JJ, et al. A randomized trial comparing telemedicine case management with usual care in older, ethnically diverse, medically underserved patients with diabetes mellitus: 5 year results of the IDEATel study. J Am Med Inform Assoc. 2009;16(4):446-56.
- Basile JN. Systolic blood pressure. BMJ. 2002;325(7370):917-8. doi:10.1136/bmj.325.7370.917
- Bundy JD, Li C, Stuchlik P, Bu X, Kelly TN, Mills KT, et al. Systolic blood pressure reduction and risk of cardiovascular disease and mortality: A systematic review and network meta-analysis. JAMA Cardiol. 2017;2(7):775-81.
- Grossman E. Blood pressure: The lower, the better: The con side. Diabetes Care. 2011;34 Suppl 2(Suppl 2):S308-12.
- Clark NG, Pawlson G. Change in HbA1c as a measure of quality of diabetes care: Response to spitz. Diabetes care. 2006;29(5):1184-5.
- Karyekar CS, Frederich R, Ravichandran S. Clinically relevant reductions in HbA1c without hypoglycaemia: results across four studies of saxagliptin. Int J Clin Pract. 2013;67(8):759-67.
- Sherwani SI, Khan HA, Ekhzaimy A, Masood A, Sakharkar MK. Significance of HbA1c test in diagnosis and prognosis of diabetic patients. Biomark Insights. 2016;11:95-104.
- Franco MR, Pereira LS, Ferreira PH. Exercise interventions for preventing falls in older people living in the community. Br J Sports Med. 2014;48(10):867-8.
- Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012;2012(9):CD007146.
- Rubenstein LZ, Josephson KR, Trueblood PR, Loy S, Harker JO, Pietruszka FM, et al. Effects of a group exercise program on strength, mobility, and falls among fall-prone elderly men. J Gerontol A Biol Sci Med Sci. 2000;55(6):M317-21.
- Feldman DI, Al-Mallah MH, Keteyian SJ, Brawner CA, Feldman T, Blumenthal RS, et al. No evidence of an upper threshold for mortality benefit at high levels of cardiorespiratory fitness. J Am Coll Cardiol. 2015;65(6):629-30.