Archive \ Volume.15 2024 Issue 2
Complications after Surgery on the Thyroid Gland: A Review
Abstract
It is recommended to perform thyroid surgery for many reasons. The most important one is to diagnose thyroid tumors through fine needle biopsy. This method remains the gold standard for evaluating nodules. There has been a significant increase in thyroid carcinoma cases in Russia in the last 15 years. This can be attributed to better and more systematic diagnosis methods that allow the detection of even very small cancers. In addition, tumors from Hurthle-cells warrant surgery, at the very least lobectomy. This is because pathohistological diagnostics is still the most reliable way to distinguish benign tumors from malignant ones. It should be noted that patients should receive proper advice regarding potential complications before any surgical intervention, they should be fully aware of all possible risks. This review looks at mild (seroma) and severe (recurrent neural damage, hypoparathyroidism, bleeding, and seroma) complications that can occur after thyroid surgery. This review examines the possibilities for treatment and prevention of each of these complications.
How to cite:
Download Citation
INTRODUCTION
The history of thyroid gland cognition has its roots in the second millennium BC when the struma was described by Chinese doctors. The endemic goiter was known to the ancient Greeks and Romans. Hippocrates, Pliny the Elder, and Marco Polo described this disease. In the 16th century, Paracelsus first drew attention to the connection of endemic goiter with cretinism and emphasized the social significance of this disease [1]. A brief description of the appearance of the thyroid gland was first given by K. Galen at the beginning of the XV century. The organ is described more fully in the works of A. Vesalius (1543). In 1836 Th. W. King was the first to put forward the concept of the intracretory activity of the thyroid gland. Claude Bernard in 1855 proved that the gland has an endocrine function and that the secret secreted by it enters the bloodstream, affecting the body. In 1835, Graves and 1840, K. Bazedov described the clinical manifestations of increased thyroid function. In 1880, Borneville described the congenital absence of the thyroid gland, calling the resulting condition myxedema. Pastor et al. made the first attempts to treat myxedema with a thyroid transplant while observing a temporary improvement in the condition [1].
Thyroid extract was first used to treat myxedema in humans in 1891 by Murray. E. Baumann in 1896 noted the close relationship between iodine intake in the body and the functional activity of the organ.
The main thyroid hormone L-thyroxine was isolated and purified by Kendall in 1915; after isolation in crystalline form and determination of the chemical structure by Harington and Berger in 1926-1927, it was possible to synthesize thyroxine. In parallel, Hershman et al. and Orloff et al. proved the presence of a second thyroid hormone, triiodothyronine [2, 3].
In the middle of the XIX century, the period of formation and development of thyroid surgery began, which is associated with the names of Reverden and Kocher. Jacques Reverden initiated thyroid surgery, and first coined the expression "mixoedeme postoperatoire".
Mixing the functions of the thyroid and parathyroid glands for a long time did not allow us to obtain objective data on the role of the thyroid in homeostasis. This led to a large number of complications resulting from surgical interventions on the thyroid gland. The discovery of epithelial bodies in humans and animals by Swedish scientist Ivar Sandstroem in 1880, as well as experimental evidence of the role of these glands in the life of the whole organism, presented in 1891 by Glei, gave a tangible impetus to the development of endocrine surgery. As known, tetany is caused not by removal of the thyroid gland, but by accidental excision of epithelial cells [2].
A huge contribution to the development of thyroid surgery was made by the Swiss surgeon, professor of the surgical clinic in Bern, Theodor Kocher. He has deeply studied the problems of asepsis and antiseptics, abdominal surgery, and traumatology. T. Kocher's research on the problems of goiter, thyrotoxicosis, goiter cretinism, iodine therapy and prevention of thyrotoxicosis, and the essence of Basedova disease are world famous. He coined the term "Cachexia thyreopriva", and developed the technique of basic operations on the thyroid gland.
In 1906, the American surgeon George Crile proposed an original surgical technique for the surgical treatment of metastases of cancer of the head and neck organs, which consisted of excision of the cervical tissue simultaneously with excision of the primary tumor. Later, the surgery technique described by Baloch et al. began to be used for metastases of tumors of the upper respiratory tract, salivary glands, and thyroid [4].
MATERIALS AND METHODS
The analysis of publications, abstracts, and texts of scientific articles in various scientometric databases was carried out using the keywords "thyroid surgery", "complications", "hypocalcemia", and "thyroidectomy". Such resources as PubMed, CyberLeninka, Hindawi, and Google Scholar were used as sources of information, while access to the materials of interest was not limited. In addition, a manual literature search was also conducted.
RESULTS AND DISCUSSION
Figure 1 shows the distribution of patients by gender based on the type of pathology.
|
|
|
Figure 1. Distribution of patients by pathology gender |
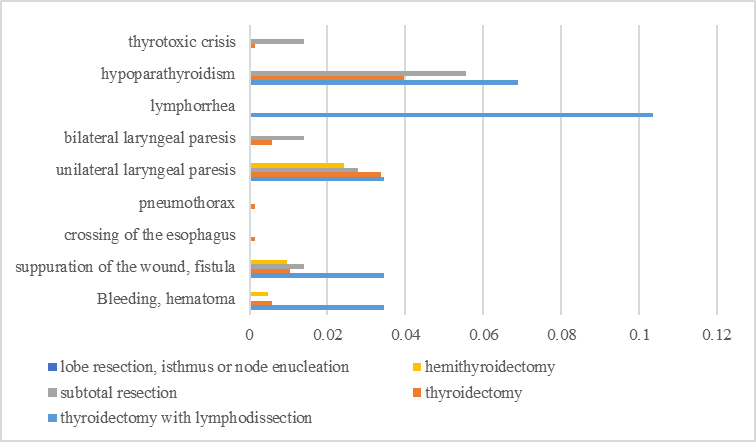
Complications after thyroid surgery can be divided into lighter and more severe. Figure 2 shows the distribution of complications depending on the volume of surgery. The milder complications of thyroid surgery include the formation of seroma and more pronounced scarring of the wound. Seroma is the accumulation of clear fluid after surgery or injury [5]. Small seromas can heal on their own without treatment; for larger ones, aspiration and drainage in sterile conditions are recommended. The formation of seroma after thyroidectomy has been studied only briefly; Apparently, the frequency of their occurrence can be slightly reduced by using newer devices such as ultrasonic coagulation knives to quickly and correctly reduce the risk of seroma formation [6]. In addition, proper drainage of the healing wound is recommended.
|
|
|
Figure 2. The prevalence of postoperative complications depends on the volume of surgery |
The aesthetic results of thyroid surgery are of paramount importance for most women and young people who undergo it. Achieving favorable aesthetic results is especially important during thyroidectomy surgery. An incision made in a prominent anatomical area on the neck should be as delicate and non-traumatic as possible. However, traditional thyroidectomy is associated with a greater risk of scarring than less popular endoscopic methods; Scars can not only be noticeable but also cause symptoms such as a foreign body sensation and difficulty swallowing. Scar tissue can spread beyond the surface of the skin into the muscles up to the thyroid cartilage (Kim) [7].
As a result of studying the risk factors for hypertrophic scar formation after thyroidectomy, it was found that protruding sternocleidomastoid muscles and a small distance between the incision and the jugular notch are associated with a higher frequency of hypertrophic scar formation [8, 9]. Insufficient attention is paid to hypertrophic scars in the scientific literature.
Since nerve fibers and blood vessels that supply muscle cells with blood can be damaged or altered, postoperative dysphagia is often associated with surgical interventions for paratracheal tumors or hyperthyroidism [10, 11]. During surgery, the most common complications of thyroidectomy are bleeding and hematomas. This is because the thyroid gland has an abundant blood supply, which increases the risk of bleeding [12]. The effects of bleeding are still unknown in clinical studies. In most cases, blood loss is caused by insufficient compression of small vessels or insufficient coagulation, spikes in blood pressure, or damage to thyroid tissue. Swelling of the neck does not always indicate severe blood loss; rather, it may indicate superficial blood loss in or under the muscle layers. Over time, hematomas can become even more dangerous as their bleeding increases; unfortunately, they often do not cause swelling of the neck, which makes them difficult to detect. Pressure can rapidly increase in a limited area of the neck, which leads to respiratory failure or hypoxia and congestion in the larynx, followed by venous-lymphatic blockage in the endotrachea. This increases breathing difficulties and the risk of hypoxia. Thus, a deep neck hematoma can be much more dangerous than one located closer to the surface, since most of them occur within 24 hours after surgery [13].
In the traditional practice of hemostasis, large vessels are ligated, and smaller vessels undergo bipolar coagulation for hemostasis [14]. This method is quite safe, and effective, and the risk of damage to nerves and parathyroid glands is minimized, unlike monopolar surgery, which should be avoided due to elevated temperatures resulting from concomitant damage, which is caused by an increased risk of bleeding [15]. It has been suggested that the use of ultrasound dissection can reduce both intraoperative and postoperative blood loss, as well as reduce thermal damage to critical structures.
Some authors, for example, recommend loosely suturing muscles with tourniquets to prevent deep hematomas. Most patients who have undergone thyroid surgery are recommended to undergo 24-hour postoperative follow-up. When stridors and shortness of breath appear in combination with the development of bleeding, an urgent reaction is necessary. The reopening of the surgical wound should be carried out as soon as possible to drain as much blood as possible, and then return the patient to the operating room for a repeat operation.
Damage to the recurrent nerve caused by laryngectomy has been reported for a long time. This branch of the vagus nerve provides all the muscles of the larynx, and the cricoid gland, except those that supply the cricoid gland. These nerves run unevenly. The left nerve is located under the segment of the aorta, and its branch runs along the subclavian vein before ending at the neck. Passing through the tracheoesophageal sulcus, the nerves connected to the thyroid gland can enter at levels close to where the cricoid gland is located in the throat. Most often, damage to the recurrent pharynx occurs near this nerve entrance to the larynx. Unilateral paresthesia causes flabbiness of one vocal fold, which leads to dysphonia, which progresses to complete paralysis of the vocal cords [16]. The consequences of repeated damage to the larynx (RLN) can become more serious over time. With unilateral damage to the laryngeal nerve, the affected vocal cords can atrophy and reduce voice quality, while bilateral damage causes closure of the glottis, which leads to biphasic stridor, respiratory distress, and possible aphonia; urgent interventions such as tracheostomy or intubation may be required as immediate treatment [17]. RLN dysfunction may occur during extubation after total thyroidectomy. However, damage does not always lead to paralysis - in the case of partial damage, symptoms can still manifest unilaterally or bilaterally, although they can usually be milder due to partial damage rather than incomplete paralysis. Such injuries can occur for a variety of reasons, including insufficient visualization during surgery, anatomical changes and bleeding during or after surgery, as well as the formation of edema. Monitoring damage to the recurrent laryngeal nerve (RLN) during surgery, even in complex cases involving cancer, large goiter, or repeated operations, is of great importance. According to studies, the frequency of irreversible nerve damage ranged from 0.5 - 5.0%, while temporary damage occurred in 1-30% of cases [18].
CONCLUSION
Modern advances in surgical techniques, hemostatic measures, and intraoperative monitoring have dramatically enhanced both safety and efficacy during thyroid surgery in recent years. Key developments include intraoperative monitoring of the recurrent laryngeal nerve and techniques for identifying and conserving parathyroid glands. Preventing complications during thyroid surgery requires an in-depth knowledge of cervical anatomy and histology. Surgeons require in-depth knowledge of the intricate structures surrounding the thyroid gland, including its nerve supply (recurrent laryngeal nerve), parathyroid glands (parathyroid glands), and their respective blood supplies. Visualization techniques play a pivotal role in accurately identifying and protecting vital structures, like nerves and parathyroid glands. Surgeons take great care during surgery to avoid inadvertent damage or removal of these essential elements. Intraoperative monitoring techniques enable real-time evaluation of nerve function and early identification of complications during surgery. Furthermore, methods like meticulous dissection and careful hemostasis help mitigate bleeding risk while simultaneously decreasing tissue trauma during procedures. Healthcare providers strive to optimize patient safety and outcomes during thyroid surgery by adhering to best practices and employing advanced surgical tools. Furthermore, patients should receive adequate consultation regarding potential complications before surgery, so that they are fully aware of all possibilities before going under anesthesia.
ACKNOWLEDGMENTS: All the authors were involved in the conceptualization, methodology, formal analysis, writing, and editing of the manuscript.
CONFLICT OF INTEREST: None
FINANCIAL SUPPORT: None
ETHICS STATEMENT: None
References
- Pastor J, Libánský P, Adámek S, Lischke R, Naňka O. History of thyroid surgery. Rozhl Chir. 2020;99(11):476-80.
- Hershman JM, Davies TF, Emerson CH, Kopp PA. Retrospective view of thyroid by its former editors. Thyroid. 2020;30(1):2-7. doi:10.1089/thy.2019.0775
- Orloff LA, Parangi S. History of thyroid surgery in the last century. Thyroid. 2023;33(9):1029-38. doi:10.1089/thy.2022.0629
- Baloch Z, LiVolsi VA. Fifty years of thyroid pathology: Concepts and developments. Hum Pathol. 2020;95:46-54. doi:10.1016/j.humpath.2019.09.008
- Dey A. Should seroma be considered a complication? Hernia. 2022;26(1):377-8. doi:10.1007/s10029-021-02385-w 8
- Nidheesh PV, Gökkuş Ö. Advances in electrocoagulation process. Chemosphere. 2023;310:136779. doi:10.1016/j.chemosphere.2022.136779
- Kim WW. Transoral thyroidectomy: Advantages and disadvantages. J Minim Invasive Surg. 2020;23(3):112-3. doi:10.7602/jmis.2020.23.3.112
- Xie H, Xiang Y, Yang E, Zhang H. Factors influencing hypertrophic scarring after thyroidectomy. Adv Skin Wound Care. 2021;34(10):1-6. doi:10.1097/01.ASW.0000775924.92065.78
- Kim BR, Kwon SH, Kim JW, Jeong WJ, Cha W, Jung YH, et al. Early postoperative injections of polydeoxyribonucleotide prevent hypertrophic scarring after thyroidectomy: A randomized controlled trial. Adv Wound Care (New Rochelle). 2023;12(7):361-70. doi:10.1089/wound.2022.0025
- Đanić-Hadžibegović A, Hergešić F, Babić E, Slipac J, Prstačić R. Thyroidectomy-related swallowing difficulties: Review of the literature. Acta Clin Croat. 2020;59(Suppl 1):38-49. doi:10.20471/acc.2020.59.s1.05
- Galluzzi F, Garavello W. Dysphagia following uncomplicated thyroidectomy: A systematic review. Eur Arch Otorhinolaryngol. 2019;276(10):2661-71. doi:10.1007/s00405-019-05599-y
- Doran HE, Wiseman SM, Palazzo FF, Chadwick D, Aspinall S. Post-thyroidectomy bleeding: Analysis of risk factors from a national registry. Br J Surg. 2021;108(7):851-7. doi:10.1093/bjs/znab015
- Ortoleva J, Drake FT, Moor A, Ortega R. Hematoma with airway compromise after thyroidectomy. Anesthesiology. 2024;140(1):142-3. doi:10.1097/ALN.0000000000004718
- Palta S, Saroa R, Palta A. Overview of the coagulation system. Indian J Anaesth. 2014;58(5):515-23. doi:10.4103/0019-5049.144643
- Czyz CN, Abramowitz BD, Goodman AE, Foster JA, Cahill KV, Everman KR. Infection rates after periocular surgery utilizing new versus re-processed monopolar electrocautery. Surg Infect (Larchmt). 2015;16(3):241-3. doi:10.1089/sur.2014.055
- Ivey CM. Vocal fold paresis. Otolaryngol Clin North Am. 2019;52(4):637-48. doi:10.1016/j.otc.2019.03.008
- Liang KY, Scharpf J. Avoiding complications of thyroidectomy: Recurrent laryngeal nerve and superior laryngeal nerve preservation. Otolaryngol Clin North Am. 2024;57(1):75-82. doi:10.1016/j.otc.2023.08.001
- Nobles ER Jr. Nonrecurrent laryngeal nerve. Arch Surg. 1970;100(6):741-2. doi:10.1001/archsurg.1970.01340240079017